Telemedicine offers the convenience of virtual appointments via video or phone, benefitting both health and ease of access. It allows healthcare providers to see patients in their home environment, giving certain specialists an advantage. Telemedicine became a lifesaver during the pandemic, with providers and patients leveraging virtual consults to maintain communication without risking physical interaction. Outsourced medical billing services stepped up to the challenge by helping providers ensure adherence to billing guidelines for telemedicine and telehealth for optimal reimbursement.


Elevate your workflow and boost financial outcomes with our medical billing services!
Call Now (800) 670-2809
Telehealth Usage Trends
According to an AMA survey of more than 1,300 physicians, more than 80% of physicians used tele visits in 2022. Nearly 70% of doctors said they want to keep providing telehealth services.
Telemedicine is evolving, also transitioning into “telehealth” to represent a variety of medical services using both synchronous and asynchronous technologies, including:
A range of providers, such as physicians, nurse practitioners, clinical psychologists, and licensed clinical social workers can offer telehealth services to their patients. Speech-language pathologists, physical therapists, audiologists and occupational therapists can also provide care via telehealth. Clinicians can deliver some non-behavioral/mental health services via audio-only telehealth.
Permanent Medicare Telehealth Changes
While the public health emergency (PHE) ended in May 2023, CMS has made certain telehealth adjustments permanent. These changes primarily revolve around mental health care:
- Geographic and originating site restrictions on Medicare telehealth services are waived beginning the day of the Public Health Emergency through December 31, 2024.
- Medicare coverage and payment for audio-only services will continue through December 2024.
- Medicare patients can receive behavioral/mental telehealth services in their homes.
- Rural health clinics and federally qualified health centers can function as distant site providers for behavioral/mental health care.
- Rural hospital emergency departments are eligible as originating sites.
- Opioid treatment programs will be able to provide counseling and therapy by phone.
Billing Guidelines for Telemedicine and Telehealth
Here are the key guidelines for billing telemedicine/telehealth:
Place of Service (POS) Codes
Use ’95’ Modifier: Continue billing telehealth claims with the POS indicator used to bill for an in-person visit. Use the “95” modifier to indicate it was a telehealth appointment.
After December 31, 2023, use POS 02-Telehealth to indicate that the billed service was provided as a professional telehealth service when the originating site is other than the patient’s home. Use POS 10-Telehealth for services when the patient is in their home.
Distant Sites
A distant site is the place where a healthcare professional conducts telehealth services. Prior to the PHE, specific categories of distant site providers were authorized to offer and receive compensation for telehealth services. Until December 31, 2024, all eligible Medicare billing providers can deliver telehealth services from a distant site.
Technology
- For behavioral or mental telehealth, you may use 2-way, interactive, audio-only technology.
- Audio-only telehealth is allowed for some non-behavioral or mental telehealth services through December 31, 2024. These services include speech therapy, nutritional counseling, and medication management.
- For most non-behavioral or mental telehealth, you must use 2-way, interactive, audio-video technology.
Codes for Billing Telehealth Encounters
Medicare added more than 100 codes for telehealth care during the PHE. Professional telehealth claims should be submitted using the appropriate CPT or HCPCS code. Here are some of the CPT codes for billing telemedicine/telehealth services:
Telephone evaluation and management codes (established patients)
The following CPT codes can be used by physicians or other qualified health professionals who may report E/M services for established patients provided via telephone:
Remote Evaluation and Virtual Check-in
The HCPCS codes to report remote evaluation and virtual check-in are:
G2010 – Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store-and-forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available.
G2012 – Brief communication technology-based service, e.g., virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment: 5-10 minutes of medical discussion.
G2252 – Brief communication technology-based service, e.g., virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment: 11-20 minutes of medical discussion.
Remote Physiological or Patient Monitoring (RPM)
RPM codes are for patients needing ongoing care like chronic, post-discharge, or senior care.
99453 – Remote monitoring of physiologic parameter(s) (e.g, weight, blood pressure, pulse oximetry, respiratory flow rate), initial set-up and patient education on use of equipment
99454 – Remote monitoring of physiologic parameter(s) (eg, weight, blood pressure, pulse oximetry, respiratory flow rate), initial device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days
99457 – QHP service; 20 minutes of Non F2F and F2F time spent in analysis and via synchronous communication with patient the findings or care plan.
99458 – Add-on code; full additional 20 minutes for services described in 99457.
Remote Therapeutic Monitoring (RTM)
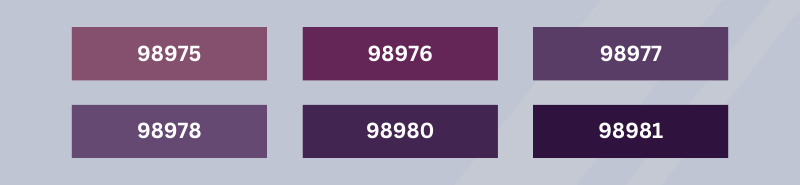
RTM monitors the progression of therapies performed by the patient based on a plan. The codes are
- 98975 – Remote therapeutic monitoring (eg, respiratory system status, musculoskeletal system status, therapy adherence, therapy response); initial set-up and patient education on use of equipment
- 98976 – Device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to monitor respiratory system, each 30 days
- 98977 – Device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to monitor musculoskeletal system, each 30 days
- 98978 – 30-day device supply with scheduled recording and/or programmed alert transmission to monitor CBT
- 98980 – Remote therapeutic monitoring treatment management services, physician or other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient or caregiver during the calendar month; first 20 minutes
- 98981 – Each additional 20 minutes (List separately in addition to code for primary procedure)
Evisit and Online Digital Evaluation/Management
While codes 99421-99423 are for practitioners who can independently bill E/M services, CPT codes 98970-98972 are for practitioners who cannot independently bill E/M services:
- 98970 – Qualified non-physician healthcare professional online assessment, for an established patient, for up to seven days, cumulative time during the 7 days; 5-10 minutes
- 98971 – Qualified non-physician healthcare professional online assessment service, for an established patient, for up to seven days, cumulative time during the 7 days; 11-20 minutes
- 98972 – Qualified non-physician qualified healthcare professional assessment service, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes

Enjoyed this article?
Explore deeper insights by checking out our blog post on the emerging trends in medical billing.
Challenges in Telemedicine Billing
The main challenges in telemedicine billing are:
- Current policies, regulations, and requirements for telemedicine are complex, evolving and subject to change. Understanding these laws can seem overwhelming due to their complexity.
- Telehealth billing rules on patient eligibility, service coding, and reimbursement differ across states. Compliance demands familiarity with state-specific requisites or limitations specific to telehealth.
- Identifying eligible services for telehealth billing requires providers to be knowledgeable about payer policies.
The Office of the Inspector General (OIG) stepped up efforts to detect potential fraud in rapidly adopted telehealth technology by collaborating with providers and MCOs, identifying billing patterns indicating wasteful errors or suspicious activity during COVID (https://oig.hhs.texas.gov). Common errors to watch out according to the OIG are:
- Billing for multiple telemedicine or telehealth services on the same client in a short period of time.
- Impossible hours – Billing for more than 24 hours in a day.
- Telephone-only services. Billing more than one E/M code a day, with a modifier 25, on a patient, leading to improper reimbursement.
- Billing for excess time – For teleservices claims paid for E/M with add-on psychotherapy services, audits found clinics billing for more time than was spent with clients for the psychotherapy services, as evidenced by the time recorded in the medical records and by their telemedicine platforms.
Telehealth Billing Best Practices
Pay attention to the following when billing telehealth services:
- Know the varying telehealth billing rules of payers and states.
- Accurate documentation and coding are crucial for prompt payment.
- Include diagnoses, service duration, and method used in documentation.
- Ensure coding aligns with the provided care and communication method.
- Differentiate non-face-to-face interactions in documentation.
- Understand rules for billing telephone-only services.
- Document and code place of service based on payer policies:
- Check Medicaid policies by state.
- Private insurers have varying POS code requirements.
- Know Medicare guidelines:
- Use applicable POS codes for in-person services.
- Apply modifier 95 for real-time telehealth.
- Verify coding modifiers for timed procedures with each insurer.
For Medicare claims, ensure that the service provided is included on the list of available codes for telehealth.
With all these challenges and evolving regulations, providers need to understand documentation and coding requirements to ensure accurate telemedicine billing. Partnering with an experienced medical billing company can help providers avoid errors and optimize reimbursement while providing virtual care.
Automation systems excel at processing straightforward claims that follow standard billing rules, but may struggle with verification of complex insurance policies. For example, when clients entrust us with the verification process, it allows them to inform patients about their complete financial responsibilities before their appointments. Additionally, our EMR/EHR systems automate the claims, but we still undertake a thorough review before sending them out. The automated process often overlooks important elements such as modifiers, which are crucial for ensuring claim reimbursement.