Revenue cycle management (RCM) in critical care comes with unique challenges that can lead to financial losses if not addressed properly. Critical care billing and coding rules and regulations regarding are complex and the process itself is tedious. The time spent on providing these services counts when it comes to payment. It is crucial to comply with payer rules and regulations, be it Medicare, Medicaid or other private insurers.
Best practices for medical coding in intensive care units involve accurate documentation, proper use of CPT codes, compliance with billing regulations, and proactive claim management to minimize denials and ensure optimal reimbursement. These challenges make outsourcing to an experienced medical billing company a practical strategy to ensure compliance, maximize physician reimbursement, and avoid insurance claim denials.
When providing critical care services, the physician/health care professional has to make highly complex decisions to assess, manipulate, and support vital system functions(s) to treat single or multiple vital organ system failure and/or to prevent further life-threatening conditions.
According to the Centers for Medicare & Medicaid Services (CMS), “critical care services must be reasonable and medically necessary … delivering critical care in a moment of crisis, or upon being called to the patient’s bedside emergently, is not the only requirement for providing critical care service. Treatment and management of a patient’s condition, in the threat of imminent deterioration; while not necessarily emergent, is required.”
How to Document Critical Care Services for Maximum Reimbursement
A precise, thorough report describing the motivation behind the critical care provided is necessary for persuading the insurance companies to reimburse the service, and reducing risk of claim denials.
- Critical care must be provided by the practitioner for a minimum of 30 minutes.
- If the service is less than 30 minutes, then it is reported using the appropriate E/M codes.
- CMS finalized the CPT codes 99291 and 99292 for reporting critical care services.
- Only the total duration of the critical care services, either continuous or aggregated, provided by critical care specialists to a single patient for a given date of service should be reported using these codes.
- For continuous critical care, the coding for services is accounted and reported for one day, even if the service crosses over after midnight.
- The non-continuous service that extends to the following days is reported as a new service.
- After the COVID-19 pandemic, teleICU is included as part of critical care billing.
- Only the care and time provided until a patient is declared brain dead must be billed.
- The practitioner must provide personal care for the patient, either at their bedside or on the floor or unit where they are housed.
- Critical care typically encompasses areas such as: coronary care unit, intensive care unit, respiratory care unit, and emergency department.
- As long as the services meet the critical care criteria and are not doubled, multiple critical care services from more than one specialist given to one patient at the same time can be reported. An AAPC blog points out that according to the CMS, “The reasonable and necessary services of each physician rendering concurrent care could be covered where each is required to play an active role in the patient’s treatment.”
- If multiple specialists of the same group provide the service:
- 99291 – Report the initial critical care provided concurrently by a single or more practitioners in the same field on the same date of services.
- 99292 – Report rest of the care provided with 99292.
- If a specialist completes the service before the given time duration (30 minutes), then the rest of the service time can be used by another specialist in the same field to continue medical care. The total time then spent by all specialists is added to report CPT code 992921. 99292 is reported only if additional 30 minutes beyond this time is given to the same patient on the same day.
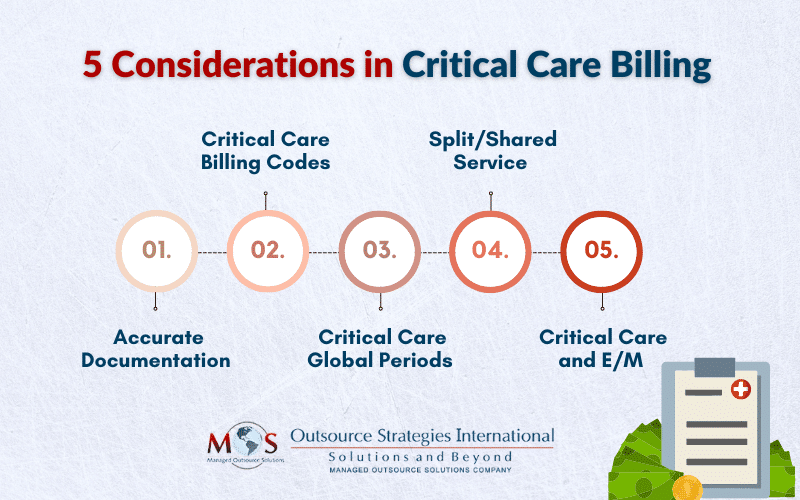
Key Considerations to ensure Accurate Billing for Critical Care Services
-
- Ensure Accurate Documentation
The basis of good critical care documentation is the provision of comprehensive information. Document high-complexity medical decision making (MDM) according to the latest methodology mentioned in the CPT book. To determine MDM, the following must be considered:
-
-
- The complexity of the critical illness(es) addressed
- The amount and/or complexity of data to reviewed and analyzed
- The risk of complications and/or morbidity or mortality
-
The provider needs to document how critical care was necessary for the patient’s condition. A blanket statement of “chest pain” and billing CPT code 99291 is inadequate for the payers. The substantive information to be included while writing a report for critical care:
-
-
- The organ system that was at risk and how it was damaged
- The deterioration in the patient’s health
- The probability of life-threatening illness
- Assessment of vital organ system
- Description of provider’s services that helped stabilize the patient’s condition
- The presence of practitioner either at the bedside or unit
- The total time spent by the practitioner furnishing critical care services
-
An ACEP FAQ provides the following example of acceptable documentation from CMS:
“Patient developed hypotension and hypoxia; I spent 45 minutes while the patient was in this condition, providing fluids, pressor drugs, and oxygen. I reviewed the resident’s documentation, and I agree with the resident’s assessment and plan of care.”
-
- Understanding CPT Codes 99291 and 99292 for Critical Care
CPT codes 99291 and 99292 are time-based service codes provided on an hourly or fraction of an hour basis. These codes represent the total duration of time spent by a physician providing critical care services, even if the time spent by the physician on that date is not continuous.
-
-
- 99291 is used to report the first 30-74 minutes of critical care
- Only once per calendar day per provider/same specialty group
- 99292 is an add-on code and used to report additional block(s) of time up to 30 minutes each beyond the first 74 minutes of critical care
- Reportable for the final 15 minutes on any given date
- Can be aggregated time met by a single physician or same group practice of the same specialty or covering provider
- 99291 is used to report the first 30-74 minutes of critical care
-
The following critical care services are included in “critical care clock time” when performed by the same physicians during critical phase and should not be billed separately.
-
-
- the interpretation of cardiac output measurements (CPT 93598)
- pulse oximetry (CPT 94760, 94761, 94762)
- chest x-rays, professional component (CPT 71045, 71046)
- blood gases, and collection and interpretation of physiologic data (e.g., ECGs, blood pressure, hematologic data)
- gastric intubation (CPT 43752, 43753)
- transcutaneous pacing (CPT 92953)
- ventilator management (CPT 94002-94004, 94660, 94662)
- vascular access procedures (CPT 36000, 36410, 36415, 36591, 36600)
-
The time spent while performing non-bundled, separately billable procedures is excluded from critical care services. Examples of common procedures that may be reported separately for a critically ill or injured patient include (but are not limited to):
-
- CPR (92950) (while being performed)
- Endotracheal intubation (31500)
- Central line placement (36555, 36556)
- Intraosseous placement (36680)
- Tube thoracostomy (32551)
- Temporary transvenous pacemaker (33210)
- Electrocardiogram – routine ECG with at least 12 leads; interpretation and report only (93010)
- Elective electrical cardioversion (92960)
-
- Critical Care Global Periods
The global surgical package includes all necessary services normally furnished by a surgeon before, during, and after a procedure. Critical care services billed separately during a global period for procedures with 10 or 90 day global period, are typically those unrelated to the surgical procedure.
Preoperative critical care may be reimbursed in addition to global fee if:
-
-
- The patient is critically ill and requires full attention of physician
- Service is unattached to specific anatomic injury or general surgical procedure performed
-
The physician’s documentation must specify the independent and distinct nature of the critical care furnished.
The modifiers that must be billed with critical care services are:
-
-
- Modifier 24 – Unrelated evaluation and management (E/M) service performed by the same physician during the postoperative period
- Modifier FT – Unrelated evaluation and management (E/M) visit during a postoperative period, or on the same day as a procedure or another E/M visit
-
Critical care during the postoperative period performed by a practitioner other than the surgeon does not require a modifier. However, CMS states in the final rule, “If care is fully transferred from the surgeon to an intensivist (and the critical care is unrelated), modifiers 54 Surgical care only and 55 Postoperative management only must also be reported.”
-
- Split/Shared Service
Effective for dates of service since January 1st 2022, critical care services are billable as split/shared evaluation and management (E/M) services. The physicians and NPP who work in the same field can split and share critical care services bill when the criteria for reporting it are met. The split shared services require modifier FS to be added.
The provider who serves the considerable amount of total time in critical care service may bill for total units of critical care. CMS defines “considerable” as “more than half the cumulative total time in qualifying activities that are included in CPT codes 99291 and 99292.” For example, if APN reports 15 minutes and MD 40 minutes then the total time equals to 55 minutes of critical care and MD is responsible for billing the visit.
An AAPC blog highlights that “To bill split (or shared) critical care services, the billing practitioner first reports CPT code 99291 and, if 104 or more cumulative total minutes are spent providing critical care, the billing practitioner reports one or more units of CPT code 99292.”
-
- Critical care and E/M
As per CMS, the same practitioner(s) in the same specialty or group can now receive payment for both critical care and E/M visits if:
-
-
- The patient was not in need of critical care when E/M service was provided
- The service is medically necessary, distinct and detached with no identical elements from critical care services provided later that date
-
When reporting these services on the claim, it is essential to append modifier 25 which is defined in CPT code set as “Modifier 25, Significant, Separately Identifiable Evaluation and Management Service by the Same Physician or Other Qualified Health Care Professional on the Same Day of the Procedure or Other Service”
Overcome Billing Challenges with Expert Support
Partnering with an experienced critical care medical billing company can help physicians comply with complex critical care documentation and billing guidelines. Such support is crucial when it comes to getting paid for high-value critical care work. Errors in billing can lead to significant financial losses, making expert revenue cycle management essential for preventing costly audits and claim denials while ensuring compliance and optimal reimbursement.


Let us handle your Critical Care billing and coding while you focus on providing exceptional patient care!