While patient care remains a top priority, the financial health of cardiology practices depends heavily on the efficiency of their Revenue Cycle Management (RCM). Ensuring accurate billing and reimbursement is one of the top challenges in the cardiology specialty. The specialty’s reliance on advanced diagnostic tests, interventional procedures, and follow-up services makes cardiology billing intricate. This post explores the top challenges in cardiology RCM and offers practical strategies to overcome them. By understanding the major cardiology medical billing challenges and implementing strategies to address them, practices can strengthen compliance, reduce claim denials, and improve financial performance. Whether you are managing a large hospital department or a private practice, understanding and optimizing your healthcare revenue cycle is essential to sustain long-term success.
Streamline your cardiology billing today
Contact our specialists to reduce denials and boost reimbursement.
Key Cardiology Medical Billing Challenges
Cardiology billing involves complex procedures, evolving payer rules, and detailed coding. Here discussed are some common challenges in cardiology medical billing and coding and how to overcome them –
- Complexity of Cardiology Billing and Coding – Incorrect CPT or ICD-10 codes, or failure to apply the right modifiers, can result in denied or delayed claims. This is one of the most significant challenges in cardiology medical billing and coding. To overcome this challenge, you can employ certified professional coders who specialize in cardiology, regularly update your coding team on CMS and payer-specific changes, and use intelligent RCM software that flags potential documentation gaps before claims submission.
- Navigating Changing Cardiology Billing Guidelines – Insurers frequently update their rules regarding cardiovascular services. Failure to keep up with cardiology billing guidelines can result in compliance risks and lost revenue. Therefore, consider assigning a compliance lead, or partner with a billing service specializing in cardiology. If performing the billing in-house, keep a central repository of payer requirements accessible to all billing staff to ensure consistent adherence.
- Documentation Gaps – Incomplete or unclear documentation is another reason for claim rejections. Without detailed records of procedures, supporting tests, and physician notes, insurers may deny or underpay claims. Standardize documentation processes and encourage physicians to capture all necessary details during patient encounters to support accurate cardiology medical billing and coding.
- Frequent Claim Denials – Due to the complexity of cardiology billing, many practices experience high claim denial rates. The reasons often include incorrect coding, lack of authorization, incomplete documentation, or missed deadlines. These denials delay revenue and increase the administrative burden. Learning how to reduce claim denials in cardiology billing is critical when it comes to sustaining cash flow. In order to overcome this challenge –
- Conduct pre-submission reviews to catch errors before claims go out.
- Implement a denial management system to track denial patterns to identify the root causes, analyze denial patterns and recurring issues.
- Establish a timely and organized appeals process.
- Conduct routine internal audits to catch issues before submission.
- Automate resubmission processes for faster turnaround.
- Compliance Risks and Payer Audits – Cardiology services are high-value and attract frequent payer audits. Missteps in coding or documentation can lead to costly penalties or repayment demands. Perform internal audits regularly and ensure staff are trained in audit triggers and payer-specific requirements. This proactive approach reduces risk and strengthens compliance.
- Inadequate Patient Data Management – Accurate patient data management is the foundation of an efficient healthcare revenue cycle. Errors in demographics, insurance details, or treatment history can disrupt billing, lead to rejections, or compromise compliance. Therefore, it is important to adopt integrated systems that sync patient records across departments. Digital intake forms can be used to reduce manual entry errors. Also, schedule routine data audits and encourage patients to review their information at each visit.
- Outdated Systems and Workflow Inefficiencies – Fragmented workflows and outdated billing systems can slow down claims processing and increase human error. Integration between your EHR and billing software is essential. Therefore, it is important to adopt billing platforms designed for cardiology practices. Features like automated coding suggestions, real-time eligibility checks, and denial tracking can streamline operations.
- Staff Turnover and Training – Many cardiology billing departments have a high turnover rate. Training new staff to meet standards and keep up with updates is tough. Lack of experience and knowledge about cardiology terms leads to coding errors. Ongoing education helps new staff improve coding skills and minimize mistakes.
Simplify cardiology medical billing challenges and maximize your practice’s revenue cycle
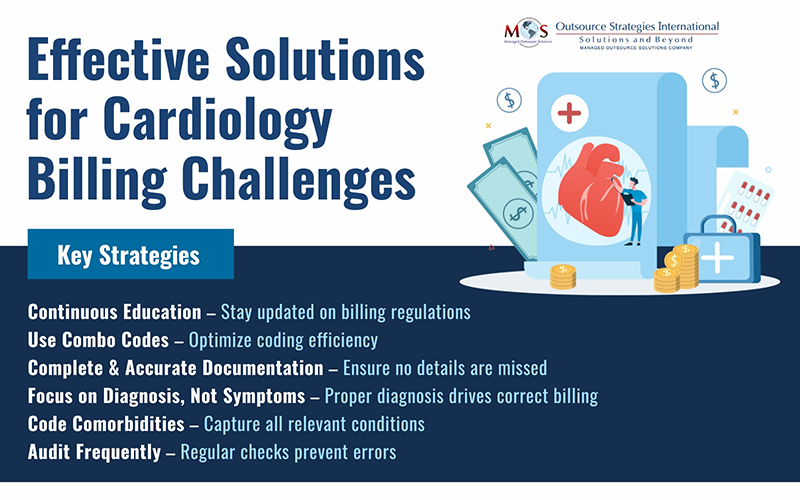
Effective Solutions to Challenges in Cardiology Billing
- Continuous Education (knowledge of coding changes) – ICD-10 and CPT codes undergo changes regularly. The medical billing and coding team must be aware of these changes. Modifiers are one of the critical components in medical coding. If there are errors in using modifiers, it will impact your revenue and result in compliance issues. The billing team must also be knowledgeable about rules and regulations related to cardiology. Staff education is therefore essential to keep the billing and coding team stay current.
- Using Combo Codes – ICD-10-CM has several combination codes for cardiology conditions. The billing team must be aware of these codes and use them appropriately to describe the patient’s condition correctly. Cardiology coders need to know and follow various coding instructions such as “Code also,” Use additional codes,” and “Code first” to give a complete picture and avoid denials.
- Complete and Accurate documentation – To ensure full payment of your cardiology claims, it is vital that documentation be complete and accurate. Incomplete documentation will quite likely result in missing codes and thus loss of revenue to the practice. In the case of procedures, documentation gaps for cardiac catheterization may lead to the loss of potential codes / codable components. This includes bifurcation interventions versus branch interventions, supplies used and additional medications used outside of the “standard.” Also, changes in the anticipated procedure may arise due to the actual condition of the patient. Hence accurate documentation is needed in cardiology.
- Focus on Diagnosis, Not Symptoms – In cardiology billing, coding should be done only when a diagnosis is confirmed. Coding for symptoms associated with disease must be avoided. However, symptoms usually not associated with an illness may be reported according to ICD-10 official guidelines.
- Coding Comorbidities – Coding comorbidities will ensure that the physician gets higher reimbursement. Documenting comorbidities helps to show the complexity of the case.
- Audit Frequently – Regular internal and external audits will reveal common coding and documentation errors. It will show up areas where the staff need to be trained. An open communication channel between physicians and the billing team is vital for successful revenue cycle management.
By understanding the major cardiology medical billing challenges – from intricate cardiology medical billing and coding to compliance with evolving cardiology billing guidelines and implementing targeted strategies – practices can streamline their billing processes. Focusing on training, accurate medical coding for cardiology, robust documentation, and proactive denial management help reduce errors and claim rejections. In short, adopting best practices in billing can help cardiology practices optimize reimbursement and maintain a strong financial foundation.




