In healthcare administration and medical billing, authorization requirements remain one of the most important yet commonly misunderstood components. Insurance companies rely on authorization to confirm whether a medical service should be covered, ensuring the procedure is both medically necessary and financially justified. Two of the most significant authorization types are prior authorization and retro authorization. While both play a role in insurance approval, their timing, purpose, and influence on reimbursement vary considerably. Understanding retro authorization vs prior authorization is crucial for providers, billing professionals, and patients who want to prevent unnecessary delays, claim denials, and financial complications.
This post outlines the key distinctions between these two authorization types, highlights their importance in medical billing, and explains how each impacts claims processing, compliance, and overall reimbursement outcomes.
What Is Prior Authorization?
Prior authorization (PA) (often referred to as pre-authorization or pre-certification) is a requirement by insurance companies for certain services, procedures, or medications to be approved before the patient receives them. Prior authorization ensures that the treatment is medically necessary and aligns with the payer’s guidelines. Insurance prior authorization is a preventive measure designed to –
- Manage healthcare costs
- Avoid unnecessary or duplicative procedures
- Ensure appropriate use of high-cost services
- Protect the payer from unexpected financial liability
For healthcare providers, completing prior authorization correctly helps secure timely reimbursement and reduces the risk of claim denials. For patients, it offers greater financial clarity. However, prior authorization can be time-consuming. Any specific delays in approval can impact patient care, while mistakes in the process can lead to claims denial and appeals that require significant administrative effort.
Optimize your authorization workflow
To reduce denials and streamline your billing process.
What Is Retro Authorization?
Retro authorization (also known as retrospective authorization) occurs when insurance approval is requested after the patient has already received medical services. This may happen for several reasons, including emergencies, oversight, or incorrect insurance information at the time of service. Retro authorization is typically considered when –
- A patient was unable to provide insurance information at the time of service
- The provider was unaware that prior authorization was required
- A situation was urgent or emergent
- There was a technical or administrative error
- The payer allows retro authorization under special circumstances
Key Differences between Retro Authorization and Prior Authorization
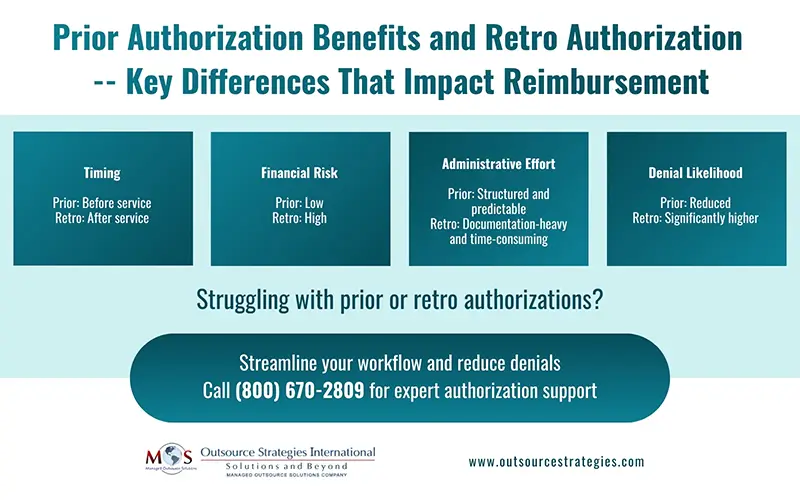
- Timing of Approval – Prior authorization is obtained before a medical service is performed, giving providers confirmation that the treatment is covered and reducing the risk of claim denials. Retro authorization is requested after the service is delivered – usually due to emergencies, missing insurance information, or administrative oversights. As care has already been provided, retro authorization carries a much higher risk of denial, making the timing of approval a crucial factor in overall reimbursement outcomes.
- Role in Emergency or Urgent Care – In true emergencies, insurers may ignore prior authorization rules to ensure immediate patient care. However, once the emergency subsides, healthcare providers may still need to request retro authorization to secure coverage. Retro authorization becomes especially relevant when treatment is delivered without the opportunity for pre-approval. Even so, approval is not guaranteed, and strong documentation proving medical necessity is essential for successful reimbursement.
- Administrative Burden – Both authorization types involve administrative effort, but retro authorization is far more labor-intensive. Prior authorization typically follows a structured process with clear guidelines, whereas retro authorization requires extensive documentation, additional communication with payers, and often detailed justification for services already rendered. Healthcare providers may need to gather medical records, submit multiple forms, and navigate lengthy back-and-forth interactions – especially if the initial retro request is denied and leads to appeals. As a result, the administrative burden associated with retro authorization is significantly greater, placing added pressure on billing teams and slowing down reimbursement.
- Level of Financial Risk – Prior authorization minimizes financial risk. Once approved, claims have a higher likelihood of being processed without issues (assuming documentation matches the request). Retro authorization, on the other hand, carries significantly higher financial risk because the service has already been performed. If the insurance company refuses retro authorization, the provider may have to absorb the cost or bill the patient.
- Likelihood of Claims Denial – Prior authorization dramatically reduces the chance of claim denial, whereas retro authorization increases it. Many claim denials occur because –
- No authorization was obtained
- The payer does not allow retro authorization
- Documentation does not support medical necessity
- Payer Policies and Flexibility – Insurance plans typically have standardized guidelines for prior authorization. In contrast, retro authorization policies vary widely and depend heavily on individual circumstances.
Prior Authorization and Retro Authorization in Medical Billing
Prior Authorization – Medical Billing Advantages
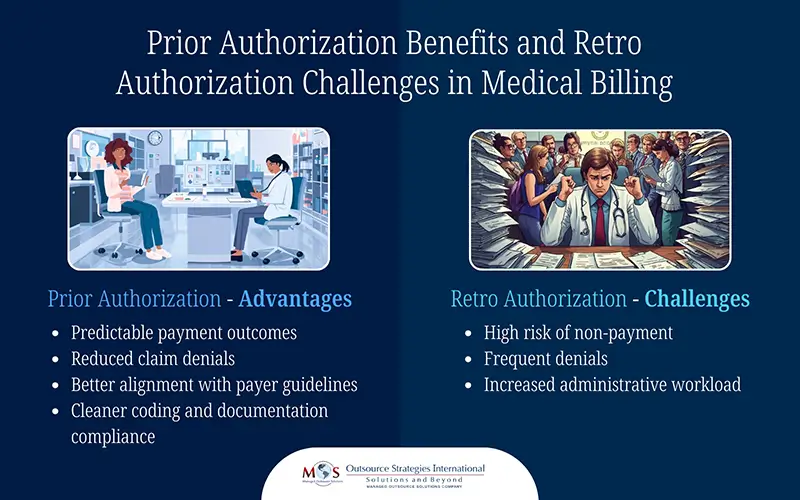
- Predictable Payment Outcomes – One of the biggest benefits of prior authorization in medical billing is the ability to secure predictable payment outcomes. When approval is obtained before treatment, providers know in advance whether the insurance company will cover the service. This point of clarity helps reduce financial uncertainty, supports accurate billing, and ensures that both the provider and patient understand the coverage details upfront. As a result, prior authorization minimizes the risk of unexpected claim issues and promotes smoother reimbursement.
- Reduced Claim Denial Rates – Prior authorization significantly reduces the likelihood of claim denials because the service has already been reviewed and approved based on medical necessity. When procedures receive pre-approval, payers are less likely to reject the claim later – unless there is a mismatch between what was authorized and what was billed. This proactive step helps prevent avoidable denials, reduces the need for appeals, and ensures more efficient revenue cycle management for healthcare providers.
- Better Alignment with Payer Guidelines – Another major billing advantage is that prior authorization ensures closer alignment with payer rules and coverage criteria. Most insurance companies have strict guidelines for high-cost or specialized services, and obtaining prior authorization allows providers to confirm that the planned treatment meets those requirements.
- Simplifies Coding and Documentation Compliance – Prior authorization helps streamline coding and documentation because the payer’s requirements are known before the service is performed. Providers can prepare accurate clinical documentation that supports the approved procedure and ensure that the billed CPT, HCPCS, or ICD-10 codes match what was authorized. This proactive alignment reduces the chance of coding discrepancies, improves overall compliance, and supports cleaner claim submissions.
Retro Authorization: Medical Billing Challenges
- Higher Risk of Non-payment – Retro authorization carries a much higher risk of non-payment because approval is sought after services have already been provided. If the payer denies the request, the provider may have to absorb the cost or bill the patient.
- Frequent Denials – Since many insurance companies have strict rules about retro authorization, these requests are often denied. Without prior approval, even medically necessary services may face rejection, leading to revenue loss.
- Increased Administrative Workload – Retro authorization requires additional paperwork, follow-ups, and communication with the insurer, making the process far more time-consuming. Billing teams often spend significant resources resolving retro-related issues.
- Dependency on Strong Medical Necessity Documentation – Successful retro authorization heavily depends on detailed medical documentation that justifies why the service was necessary. Without robust records, approval is unlikely, increasing the chance of denied claims.
Need expert help navigating retro and prior authorizations?
For end-to-end insurance support
Medical Billing and Coding Compliance Considerations
Compliance plays a huge role in both authorization types. Accurate coding, proper documentation, and adherence to payer rules are needed to secure approval. Failure to comply may lead to denials or even audits. Healthcare providers need to ensure –
- Documentation supports medical necessity
- CPT, ICD-10, and HCPCS codes reflect the service performed
- Authorization matches the billed procedure
- Records are complete and submitted on time
Retro authorization requests, in particular, require exceptionally strong documentation to justify services already provided.
Understanding the key differences between retro authorization and prior authorization is vital for maintaining efficient healthcare operations. While prior authorization is a proactive process that promotes predictable reimbursement, retro authorization is reactive, risky, and often difficult to secure.
Through strong insurance coverage verification, accurate documentation, and consistent medical billing and coding compliance, healthcare providers can minimize the need for retro authorization and ensure smoother billing workflows. Ultimately, the impact of retro vs prior authorization on claim reimbursement highlights why healthcare organizations should prioritize prior authorization processes whenever possible.
Need Help With Authorizations?
Optimize your workflow and reduce denials.
For expert retro & prior authorization support