Most women with breast cancer choose mastectomy, the surgery to remove all breast tissue (including the nipple and the areola) from one or both breasts. Primarily performed to treat or prevent breast cancer, mastectomy is normally carried out to remove existing cancerous cells within the breast and thereby reduce the potential for breast cancer to spread. The procedure is often done when a woman cannot be treated with breast-conserving surgery (lumpectomy), in which only the tumor is removed from the breast. Deciding between a mastectomy and lumpectomy can be difficult and hence women with breast cancer can decide along with their surgeon whether to be treated with a lumpectomy or a mastectomy. Oncologists and plastic surgery specialists performing mastectomy and other treatment procedures must report the same on their medical claims using the correct medical codes. Physicians should have essential medical billing and coding know-how and use the correct diagnosis and procedure codes to ensure correct and timely reimbursement.

OSI’s medical coding services will ensure that your claims are processed promptly.
Call (800) 670-2809 for more information about our mastectomy coding services!
ICD-10 Codes
- Z90.1 – Acquired absence of breast and nipple
- Z90.10 – Acquired absence of unspecified breast and nipple
- Z90.11 – Acquired absence of right breast and nipple
- Z90.12 – Acquired absence of left breast and nipple
- Z90.13 – Acquired absence of bilateral breasts and nipples
CPT Codes
- 19301 – Mastectomy, partial (e.g., lumpectomy, tylectomy, quadrantectomy, segmentectomy)
- 19302 – Mastectomy, partial (e.g., lumpectomy, tylectomy, quadrantectomy, segmentectomy); with axillary lymphadenectomy
- 19303 – Mastectomy, simple, complete
- 19304 – Mastectomy, subcutaneous
- 19305 – Mastectomy, radical, including pectoral muscles, axillary lymph nodes
- 19306 – Mastectomy, radical, including pectoral muscles, axillary and internal mammary lymph nodes (Urban type operation)
- 19307 – Mastectomy, modified radical, including axillary lymph nodes, with or without pectoralis minor muscle, but excluding pectoralis major muscle
A mastectomy may be a treatment option for many types of breast cancer, including – Ductal carcinoma in situ (DCIS), Stages I and II (early-stage) breast cancer, Stage III (locally advanced) breast cancer (after chemotherapy), inflammatory breast cancer (after chemotherapy), Paget’s disease of the breast and locally recurrent breast cancer. However, in some cases, the procedure may also be performed for reasons not related to a diagnosis of breast cancer, wherein a person suffers – severe chronic breast pain, fibrocystic breast disease, dense breast tissue and a cancer phobia or a family history of breast cancer.
Procedure and Risks
Typically, a mastectomy is performed under general anesthesia and hence patients are not completely conscious during the surgery. The procedure begins with your surgeon making an elliptical incision around your breast. The breast tissue is removed and, depending on your procedure, other parts of the breast also may be removed. An intravenous (IV) line is used to administer medicines that may be required during surgery.
There are different types of mastectomy to deal with different medical situations which include – total (simple) mastectomy, double mastectomy, skin-sparing mastectomy, nipple-sparing mastectomy, modified radical mastectomy and radical mastectomy. The type of mastectomy procedure performed will depend on a wide range of factors such as age of the patient, size, stage and grade of the tumor, menopause status, the involvement of lymph nodes and the general health of the patient. The potential risk factors include –
- Pain
- Swelling (lymphedema) in your arm if you have an axillary node dissection
- Shoulder pain and stiffness
- Numbness, particularly under your arm, from lymph node removal
- Infection
- Formation of hard scar tissue at the surgical site
- Buildup of blood in the surgical site (hematoma)
- Bleeding
Regardless of the type of mastectomy done, the breast tissue and lymph nodes that are removed will be sent to a laboratory for analysis.
Preparing for Mastectomy
Before undergoing mastectomy, patients need to meet their surgeon and anesthesiologist to discuss about the surgery (including the reasons for and risks of the surgery) and determine the plan for your anesthesia. An important point to discuss is that whether patients require breast reconstruction to be done immediately after their mastectomy, while being still anesthetized. For patients who are undergoing breast reconstruction at the same time as a mastectomy, it is important to consult a plastic surgeon before the surgery.
Plastic surgery specialists and oncologists performing breast reconstruction after mastectomy must use the relevant diagnosis and procedure codes to bill the procedure. The CPT codes for breast reconstruction surgery postmastectomy include –
CPT Codes
- 11920 – Tattooing, intradermal introduction of insoluble opaque pigments to correct color defects of skin, including micropigmentation; 6.0 sq cm or less
- 11921 – Tattooing, intradermal introduction of insoluble opaque pigments to correct color defects of skin, including micropigmentation; 6.1 to 20.0 sq cm
- 11922 – Tattooing, intradermal introduction of insoluble opaque pigments to correct color defects of skin, including micropigmentation; each additional 20.0 sq cm, or part thereof (List separately in addition to code for primary procedure)
- 11970 – Replacement of tissue expander with permanent prosthesis
- 11971 – Removal of tissue expander(s) without insertion of prosthesis
- 15777 – Implantation of biologic implant (acellular dermal matrix) for soft tissue reinforcement (breast, trunk) (List separately in addition to code for primary procedure)
- 19316 – Mastopexy
- 19324 – Mammaplasty, augmentation; without prosthetic implant
- 19325 – Mammaplasty, augmentation; with prosthetic implant
- 19330 – Removal of mammary implant material
- 19340 – Immediate insertion of breast prosthesis following mastopexy, mastectomy or in reconstruction
- 19342 – Delayed insertion of breast prosthesis following mastopexy, mastectomy or in reconstruction
- 19350 – Nipple/areola reconstruction
- 19355 – Correction of inverted nipples
- 19357 – Breast reconstruction, immediate or delayed, with tissue expander, including subsequent expansion
- 19361 – Breast reconstruction with latissimus dorsi flap, without prosthetic implant
- 19364 – Breast reconstruction with free flap
- 19366 – Breast reconstruction with other technique
- 19367 – Breast reconstruction with transverse rectus abdominis myocutaneous flap (TRAM), single pedicle, including closure of donor site
- 19368 – Breast reconstruction with transverse rectus abdominis myocutaneous flap (TRAM), single pedicle, including closure of donor site; with microvascular anastomosis (supercharging)
- 19369 – Breast reconstruction with transverse rectus abdominis myocutaneous flap (TRAM), double pedicle, including closure of donor site
- 19380 – Revision of reconstructed breast
- 19396 – Preparation of moulage for custom breast implant
- 19499 – Unlisted procedure, breast
When preparing for mastectomy, patients must follow certain instructions from the physicians and these include –
- Inform your physicians about the medications, vitamins or supplements that you are consuming, (as some substances can directly interfere with the surgery).
- Stop consuming medications a week before surgery as these can increase the risks of excessive bleeding. Medications include – aspirin, ibuprofen (Advil, Motrin IB, others) and other pain relievers, and blood-thinning medications (anticoagulants), such as warfarin (Coumadin, Jantoven).
- Don’t eat or drink 8 to 12 hours before surgery.
Don’t let coding errors delay your mastectomy reimbursements.
Partner with OSI today. Talk to us at (800) 670 2809
Recovery after the Procedure
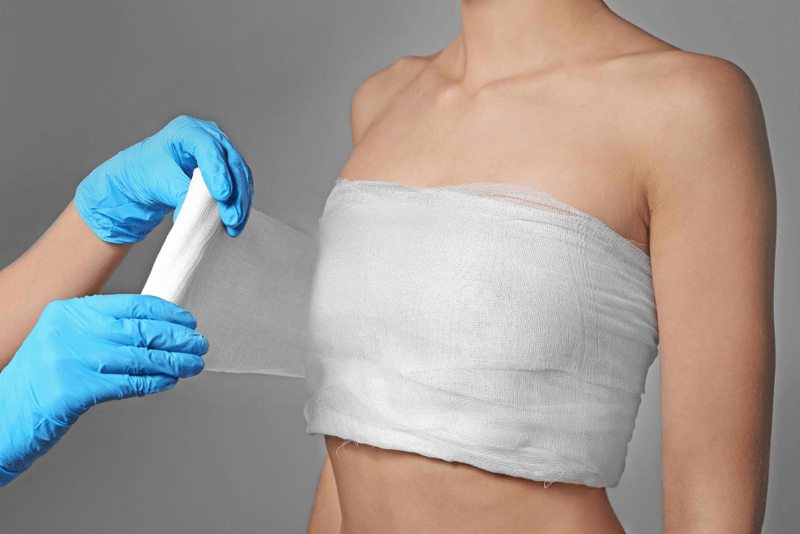
As soon as the mastectomy procedure is complete, the patient will be closely monitored wherein their heart rate, blood pressure, level of pain and feelings of nausea will be evaluated and medicated as appropriate. The average period of hospital stay after the procedure is generally 3 days. However, if reconstructive surgery is completed in the same surgery, the time of hospital stay may be slightly longer. Patients will be offered general guidelines on several issues like pain medications, care for dressings, bandages and surgical drain (if provided), signs of infection and lymphedema, when to resume wearing a normal bra or start using a prosthesis and type of exercises to minimize stiffness and scar formation to be followed during the recovery period.
The time of recovery will differ from one individual to another and may depend on the type of procedure performed. In most cases, patients can resume normal work within 3-6 weeks. However, the recovery time will be longer if reconstruction is performed along with the same mastectomy procedure as there will be high chances of pain, bruising and swelling.
Medical billing and coding can be complex and a high level of knowledge regarding appropriate coding, modifiers and payer-specific medical billing are essential for correct and on-time reimbursement. With all the complexities, the support of an experienced medical coding service provider can be useful for reporting mastectomy procedure correctly for optimal reimbursement. Professional coders in reliable medical coding outsourcing companies can ensure accurate reporting of diagnostic and procedure details.