Healthcare policies and reforms are ever-changing, so it is important to keep up with this changing landscape with effective RCM (Revenue Cycle Management) strategies. Medical practices need to streamline their administrative operations so that financial outcomes can be maximized. Lack of an optimized revenue cycle can lead to common pitfalls that every healthcare provider has to deal with. A fiscally responsible medical practice has to ensure excellent delivery of patient care along with the monitoring of overall financial health. With the implementation of ICD-10 codes and value-based reimbursement, there is voluminous patient data that has to be accounted for billing purposes. The evolving pattern of patient payment systems has increased the hassle of accurate medical billing.
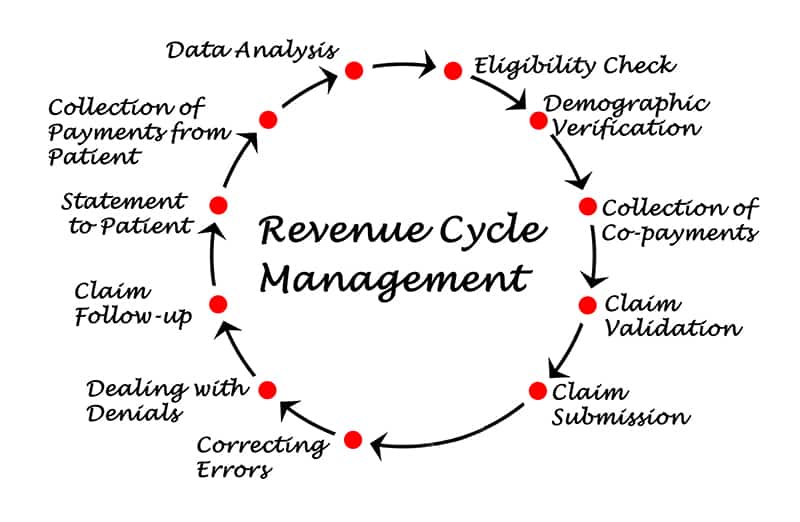
Functions that form the revenue cycle management of a hospital are:
- Documentation
- Entering demographic details of the patient
- Checking the eligibility of insurance claims
- Medical billing and coding
- Filing of the claims
If there is no seamless coordination between different units like the department of billing and coding, data analytics department, collections department and payer enrollment department, the following problems can arise:
- Non-clinical insurance claim denials that happen due to erroneous entering of patient data during registration.
- Erroneous documentation of medical codes can lead to denial of insurance payment.
- Inconsistencies in patient-provider communication due to lack of digitization impact interoperability.
- Unintentional non-compliance of Healthcare Information Portability and Accountability Act 1996 (HIPAA).
With effective troubleshooting techniques in place, medical billing and coding companies can help overcome these challenges. But the problem lies in the fact that healthcare facilities are unaware of these anomalies and proceed with the conventional methodology of management.
Below given are the lapses healthcare facilities have to avoid. These mistakes can adversely affect the revenue management cycle.
1. Lack of proper training of employees
- Medical billing requires capturing information accurately. However, human error at this stage can be the reason for the increasing number of claim denials. Unskilled staff enters the wrong ICD-10 and CPT codes corresponding to the diagnoses and treatments provided. Even missing items in the patient data and entering of wrong dates during chart documentation can lead to claim denials. This means the healthcare provider has to rework the claims, and this would delay the reimbursement.
2. Relying on existing staff strength
- When healthcare facilities depend upon the existing staff levels, it may be difficult to handle the increasing number of patients and associated data. It is important to hire the right people with the right skills. But healthcare facilities try to stretch the potential of the available staff. This negatively affects the administrative and clinical functions of the revenue cycle.
3. Fragmented administrative team
- There will be no coordination between the business and clinical sides as they prioritize different functions. The administrative task of the front-end office is to expedite claims by ensuring that the patient’s name, insurance provider and other personal information are correctly documented. The clinical function gives emphasis to the treatment received by the patient and the compilation of health care data. However, they won’t be functioning in a synchronous manner, and if there is no seamless workflow there will be mounting claim denials.
4. Failure to monitor patient’s medical claim status
- Healthcare practices don’t give importance to tracking the entire claims processing. If the potential problems in the claims are not detected, it can result in lagging accounts receivable and excessive administrative costs.
5. Skipping patient eligibility verification
- Healthcare providers must take special care to verify the eligibility of the patient prior to providing treatment. If the insurance coverage of the patient is not cross-verified, the claim will be denied. Evaluating patient eligibility plays a key role in the effective management of the revenue cycle.
6. Not leveraging new technology and trends
- Many healthcare facilities are stuck with conventional methods of billing which may not be efficient enough to handle large volumes of patient data. The inability to streamline digital workflow complicates the revenue cycle. Hospitals may not be having the adequate infrastructure or might be dealing with budget constraints. Integrating advanced technology in healthcare organizations saves time, money and effort. This, in turn, enhances ROI.
7. Not having a proactive approach to patient payments
- Medical practices hesitate to reach out to patients for their statements as an outbound calling strategy. Patients might be in need of information regarding the payments. However, if they are contacted in an active and gentle manner, medical practices can drive more patient payments. Patients can be nudged into action by creating a customized plan.
For efficacious revenue cycle management, healthcare practices have to adapt to the changing healthcare landscape. Medical billing and coding services can keep you abreast with these changes by efficiently managing the revenue cycle to maximize profit. It is because proper execution of billing and coding is necessary to considerably reduce claim denials, and this sets the foundation for successful revenue cycle management.