- What Is Retro Authorization and Why it Matters
- Different Types of Authorization in Medical Billing
- How Does Retro Authorization Work?
- Challenges in Managing Retro Authorizations
- Key Considerations and Best Practices for Effective Retro Authorization Management
- Factors Affecting Retro Authorization Eligibility in Healthcare
- The Financial Implications of Retro Authorization in Medical Billing
In the highly regulated environment of medical billing, retro authorization management is a critical process that directly impacts provider reimbursement, patient care continuity, and the financial health of healthcare practices. When prior approval is not obtained before delivering a service, retro authorization allows providers to request approval after providing treatment. Understanding how retro authorization works, when it applies, and implementing efficient processes for managing retro authorizations are essential for preventing revenue loss and minimizing claim denials.
What Is Retro Authorization and Why it Matters
Retro authorization, sometimes referred to as retrospective authorization, is a payer approval obtained after a patient has already received care. While prior authorization should always be the first line of action, there are several situations where providers legitimately rely on retro authorization –
- Emergency or urgent medical situations where delaying treatment would harm the patient.
- Administrative oversights, such as staff errors or misinterpretation of prior authorization requirements.
- Insurance changes, where updated coverage information is not available at the time of service.
- Delays from payers when providers have submitted pre-authorization requests but approval was still pending when treatment became necessary.
As these scenarios are inevitable in real-world healthcare settings, the importance of retro authorization in healthcare cannot be overstated. Retro authorization allows providers to secure reimbursement, avoid uncompensated care, and ensure that patients are not burdened financially due to circumstances beyond their control.
Optimize Your Retro Authorization Process Today
Protect Revenue and Reduce Denials.
Call Us Now!
Different Types of Authorization in Medical Billing
There are three main types of authorization in medical billing – pre-authorization, concurrent authorization, and retro authorization.
- Prior Authorization – Also called pre-authorization, this is the most common type of authorization in medical billing. It requires approval from the insurance company before a service is rendered to the patient.
- Concurrent Authorization – This involves requesting authorization for services that are already in progress. This typically occurs when a patient has an extended hospital stay or ongoing treatment.
- Retro Authorization – This allows providers to request authorization after a service has already been provided. This is typically used in emergencies or when there is a delay in obtaining prior authorization.
These different types of authorization aim to ensure that healthcare providers are appropriately reimbursed for their services and prevent any financial loss.
How Does Retro Authorization Work?
Retro authorization works by allowing healthcare providers to request authorization for services already provided to a patient. The provider submits a request to the insurance company, including all relevant information such as the patient’s medical records and the reason for requesting retro authorization. This process is crucial in instances where services were not pre-authorized, providing a mechanism to retrospectively gain approval and secure reimbursement.
The typical retro authorization workflow –
- The Patient Receives the Service – This often occurs in emergencies, urgent care scenarios, or when insurance details are unclear. Providers must act quickly to deliver care, even if authorization has not yet been established.
- Collection of Documentation – Once treatment is completed, the billing or administrative team gathers all essential documentation, including –
- Medical necessity justification
- Detailed physician notes
- Diagnostic findings, lab results, or imaging reports
- Procedure details, CPT/ICD codes, and treatment dates
- Explanation of why prior authorization was not secured
Accurate and complete documentation is the cornerstone of successful retro authorization management.
- Submission to Payer – The retro authorization request, along with supporting records is submitted to the insurance payer. Each payer has its own rules, forms, and time limits, with some requiring submission within 30–45 days of service. Missing these deadlines can lead to automatic denials.
- Payer Review – The insurer evaluates the retro authorization request by examining – medical necessity, documentation quality, accuracy of coding and validity of the explanation for lack of prior authorization. This stage determines whether the services will be reimbursed.
- Approval or Denial – Once the review is complete, the payer decides –
- Approval results in reimbursement, even though prior authorization was not obtained.
- Denial may require appeals or additional documentation. In some cases, the provider may have to write off the charges if the payer does not accept retro requests.
Get Expert Retro Authorization Management.
Challenges in Managing Retro Authorizations
Retro authorization is associated with significant challenges that can impact reimbursement timelines, revenue cycle efficiency, and overall practice productivity.
- Variability in Payer Requirements – Not all insurers accept retro authorization, and those that do often have different guidelines. Lack of standardization makes it difficult for billing teams to maintain consistency.
- High Risk of Claim Denial – Retro requests undergo stricter scrutiny, and payers may deny approvals due to – missing documentation, incorrect coding, poor justification for lack of prior authorization and submissions outside the allowed timeframe. Therefore, claims denial prevention must be a top priority in retro authorization workflows.
- Administrative Burden – Managing retro authorizations requires coordination between clinical and billing teams. Gathering medical records, communicating with payers, and tracking submission timelines can be labor-intensive.
- Delayed Reimbursement – Since services are already rendered, revenue is at risk until approval is obtained. Slow processing times can impact cash flow, especially for smaller practices.
- Lack of Awareness or Training – Staff unfamiliarity with prior authorization requirements may contribute to unnecessary retro authorization scenarios. Proper training can reduce these occurrences significantly.
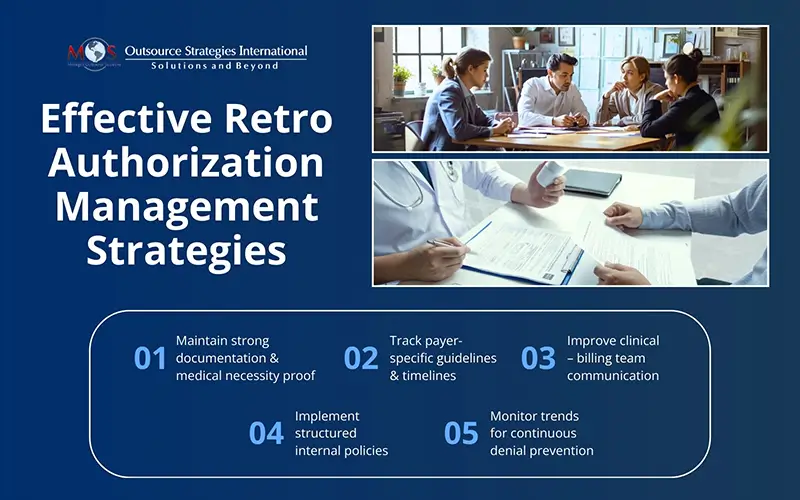
Key Considerations and Best Practices for Effective Retro Authorization Management
Healthcare organizations that excel in managing retro authorizations follow structured processes and maintain strong communication between clinical and billing teams. Below are essential best practices:
- Build Clear Internal Policies – Define situations that qualify for retro authorization. Emergency cases and payer delays should be clearly categorized. Staff should know exactly when and how to initiate the retro authorization workflow.
- Strengthen Documentation Practices – Comprehensive documentation increases approval chances. Medical necessity must be clearly supported by clinical notes, test results, and treatment rationale.
- Maintain a Payer-specific Authorization Database – Create an internal guide that outlines –
- Which payers accept retro auth
- Required documentation
- Submission deadlines
- Special requirements (forms, portals, codes)
This helps teams work efficiently and reduces avoidable denials.
- Improve Interdepartmental Communication – Smooth coordination between clinical providers and billing staff is essential. Ensure that clinical teams alert billing teams immediately when retro authorization may be required.
- Invest in Staff Training – Educating staff on prior authorization requirements reduces dependence on retro authorizations. Training should include –
- Identifying services that need pre-auth
- Understanding payer policies
- Verifying insurance coverage early
- Track and Analyze Retro Authorization Denials – Denial trends offer valuable insight. Use this data to improve documentation, identify training gaps, refine workflows and improve future approval rates.
Factors Affecting Retro Authorization Eligibility in Healthcare
Several critical factors determine whether a provider qualifies for retro authorization in healthcare. One of the most important requirements is timely submission, as most payers mandate that retro authorization requests be filed within 30 days of the service date. Insurers also conduct thorough medical necessity evaluations to confirm that the treatment was essential and appropriate.
Additionally, plan-specific limitations – such as restrictions on certain procedures or services – can influence eligibility. Provider qualifications, including compliance with state regulations and alignment with specialty requirements, also play a key role. By understanding and adhering to these criteria, providers can streamline the retro authorization process, minimize denials, and create a more efficient pathway for retro referrals.
The Financial Implications of Retro Authorization in Medical Billing
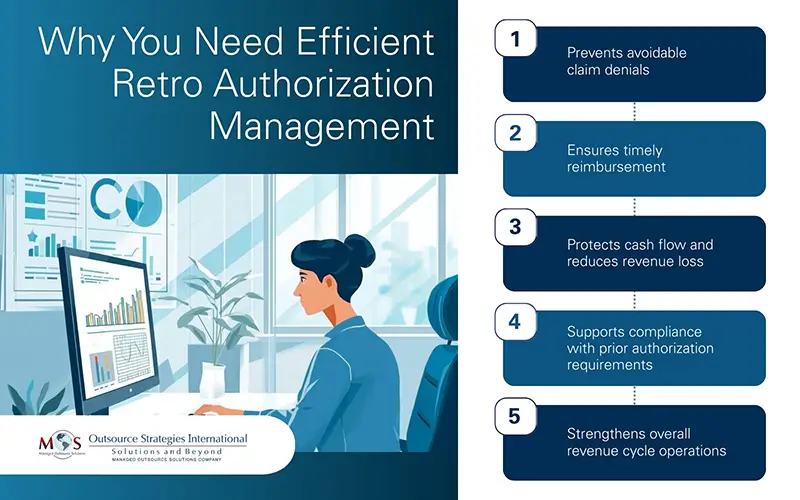
The financial dynamics of medical billing are closely tied to the effectiveness of retro authorization management. When retro authorization is delayed, incomplete, or mishandled, it can interfere with the efficiency of Revenue Cycle Management (RCM). Key financial impacts include –
- Delayed Revenue Recognition – Waiting for retro authorization approval can slow down reimbursement timelines, pushing revenue realization further out.
- Increased Administrative Burden – Staff must spend additional time gathering documentation, communicating with payers, and preparing appeals, resulting in higher operational costs.
- Potential Revenue Loss – If retro authorization is denied or submitted late, providers may face write-offs or uncompensated services.
- Effect on Cash Flow – Prolonged approval cycles and denied claims disrupt cash flow, making financial planning and day-to-day operations more challenging.
Overall, the financial implications of retro authorization stretch far beyond delayed payments. They affect every stage of the billing cycle by increasing administrative workload, risking revenue losses, and creating significant cash flow challenges.
Retro authorization is not merely an administrative backup plan; it is a strategic component of modern medical billing. Understanding how retro authorization works, strengthening documentation, and aligning workflows with payer requirements can improve approval rates and reduce financial risk. Effective retro authorization management ensures that healthcare providers receive fair reimbursement while maintaining high standards of patient care. With proper processes, training, and communication in place, healthcare organizations can navigate retro authorizations confidently – minimizing denials, optimizing revenue cycles, and reinforcing their commitment to patient-centered care.
Take Control of Your Retro Authorization Workflow.