Pain is one of the most common issues treated in hospital emergency departments (EDs). The Centers for Disease Control and Prevention estimates that 50 million Americans (or about 20 percent of the adult population in the U.S.) experience chronic pain. Interventional pain management involves the use of pain blocking techniques to treat pain and make life easier for patients. Interventional pain management services include epidural injections, epidural blocks, facet injections, discographies, nerve blocks, and spinal cord stimulation. Facet joint injection techniques are both a diagnostic tool for pain originating in these joints as well as a reliable option to treat this pain. Outsourcing medical billing can ensure correct reporting of services in compliance with coding policies and payer rules.
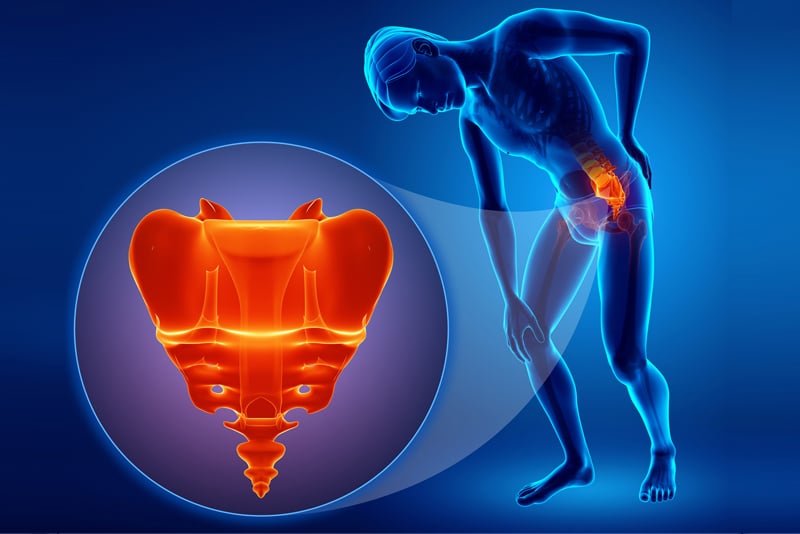
Facet joints are the connections between the bones of the spine. Pain that originates from one or more facet joints is called facet joint syndrome. The condition is caused by the degenerative changes in the facet joints. The pain usually occurs as a diffuse, dull ache in the low back and can radiate to the buttocks. Facet joint syndrome also causes pain in the neck and shoulders.
The pain can be chronic or occur as periodic flare-ups, and can be localized, referred or radiating. Joint stiffness is a common symptom of the lumbar facet pain caused by arthritis, and is typically worse in the mornings or after a long period of inactivity. Facet syndrome pain improves with moving around. However, pain can occur due to movements such as bending backwards or twisting sideways towards the affected joint.
Causes
Facet joint syndrome can affect both men and women, especially those prone to arthritis. The condition usually manifests between the ages of 40 and 70. The common causes of facet syndrome are:
- Degenerative changes in the cervical, thoracic and lumbar spine increases stain and loads on the facet joints
- Trauma like a whiplash injury of the neck
- Abnormal postures that stress the spinal tissues and the facet joints
- Repetitive movements, obesity, and poor posture and other conditions that affect the alignment of the facet joints
Diagnosis
Clinical evaluation and medical imaging and/or diagnostic injection tests are used to diagnose facet joint pain. The patient will be asked about when the pain began, duration and types of signs and symptoms; associated medical conditions, medications used, and/or surgical history. The clinical exam would include visual inspection of the affected site, hand-on inspection, range of motion tests, evaluation of each spinal segment, and a neurological exam to test muscle strength, reflexes and sensation.
Imaging (radiographs, MRI, CT, SPECT scans) may be ordered to help in the diagnosis and to identify or rule out other problems such as tumors and cysts in the lumbar spine. However, history, physical exam and imaging do not have the capability to confirm facet joint syndrome. Diagnostic facet joint injection techniques can indicate facet joints as the source of chronic spinal pain.
A diagnostic facet joint injection, also called medial branch block, is placed near a nerve leading from the suspected facet joint. Diagnostic blocks usually include local anesthesia with or without steroids injections. If the pain diminishes during the anesthetic phase of the injection, a presumptive diagnosis may be made that the pain is originating from the facet joint. This can determine if a facet joint injection might relieve your pain. Diagnostic injections are performed with either fluoroscopy or CT.
Using a double-block technique can avoid false-positive test results. The double-block technique involves administering a second facet joint block injection in the facet(s) using local anesthetics with different durations of action (e.g., lidocaine and bupivacaine). Experts say that for a positive test result, the patient must have greater than 80% pain relief for an appropriate period with each anesthetic (www.spine-health.com).
Facet Joint Syndrome Treatment Options
Self-care for facet joint syndrome include applying heat therapy, cold packs, maintaining good posture to support the lumbar curve, using a supportive brace, avoiding activities that strain the spine, staying active and doing low-impact exercises. Medical treatments recommended would include physical therapy, medications, TENS therapy and therapeutic facet joint injections. Three common injection techniques for facet joint pain are:
- Facet joint injections: These injections are delivered into the capsule that surrounds the joint to treat pain emanating from it.
- Medial branch blocks: These nerve blocks involve injecting medication around the pain transmitting medial branches of spinal nerves.
- Radiofrequency ablation (RFA): This injection treatment induces a heat lesion on the pain-transmitting nerve near the facet joint, which prevents the nerve from sending pain signals to the brain. RFA is usually considered when pain is accurately diagnosed via the the diagnostic double block injection technique.
CPT Codes for Facet Joint Injections
Compliance with coding and billing guidelines is of crucial importance in interventional pain medicine practices. The facet joint injections procedural codes are as follows:
0213T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; third and any additional level(s) (List separately in addition to code for primary procedure)
0214T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; second level (List separately in addition to code for primary procedure)
0215T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; third and any additional level(s) (List separately in addition to code for primary procedure)
0216T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; single level
0217T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; second level (List separately in addition to code for primary procedure)
0218T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; third and any additional level(s) (List separately in addition to code for primary procedure)
64490 Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophysial) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), cervical or thoracic; single level
64491 Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophysial) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), cervical or thoracic; second level (List separately in addition to code for primary procedure)
64492 Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), cervical or thoracic; third and any additional level(s) (List separately in addition to code for primary procedure)
64493 Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral; single level
64494 Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral; second level (List separately in addition to code for primary procedure)
64495 Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral; third and any additional level(s) (List separately in addition to code for primary procedure)
64633 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); cervical or thoracic, single facet joint
64634 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); cervical or thoracic, each additional facet joint (List separately in addition to code for primary procedure)
64635 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); lumbar or sacral, single facet joint
64636 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); lumbar or sacral, each additional facet joint (List separately in addition to code for primary procedure)
64640 Destruction by neurolytic agent; other peripheral nerve or branch
Points to note when billing facet joint injections: An AAPC report provides the following guidelines for imaging:
- Do not bill separately for image guidance when reporting facet joint codes
- If ultrasound guidance is used for the above procedures, the facet joint injection should be reported using 0213T-0218T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance
- If no imaging is used, 20552-20553 Injection(s); single or multiple trigger point(s)…should be reported.
The codes for facet joint injections have changed frequently over the years. Partnering with an experienced medical billing company is a practical option for interventional pain management specialist to report the correct codes to describe services rendered and ensure error-free claim submission for optimal reimbursement. Providers should ensure that documentation supports evidence of conservative management rendered as well as the site and number of injections and number of muscles.