It can be a challenge to run a successful practice while also providing high quality patient care. In order to thrive in an increasingly competitive market, your medical practice needs to adopt innovative strategies. At the heart of every successful healthcare organization is an efficient Revenue Cycle Management System (RCM). RCM begins when a patient registers an appointment to seek medical advice and ends when you have collected all claims and balance payments from patients.
Outsourcing your RCM system to a reliable medical billing services provider can help take your practice to the next level. It helps optimize every step of the complete revenue cycle to minimize operational costs and increase revenue. Leave the administrative work in the hands of experienced professionals and focus on patient care and developing your practice.
Streamline your revenue cycle and boost your financial performance with our expert medical billing services!
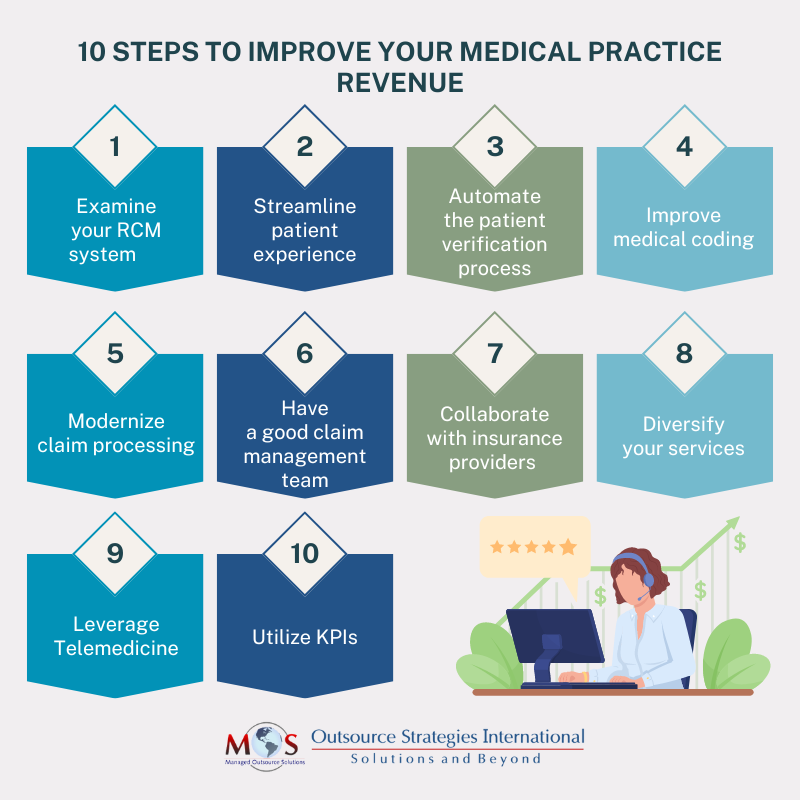
Effective Strategies That Can Help You Maximize Practice Revenue
Let’s explore effective strategies that can help you maximize practice revenue:
- Examine your current RCM system:
Evaluate your existing RCM system for a comprehensive understanding of your practice’s financial performance, current challenges, and areas that need improvement. Using this data and analyzing the workflow is critical to see what money goes out through overhead expenses, fixed costs, inefficiencies in billing or coding or claim processing and other miscellaneous expenses.
The indicators you get by monitoring statistics set a benchmark that can measures your practice’s performance against ideal performance and identifies departments that need improvement. Better revenue cycle management leads to better bottom-line for your business. Some of the metrics include:
- Aged Accounts Receivable(A/R) rate
- Bad debt rate
- Charge lag
- Days in accounts receivable
- Discharge not submitted to payer (DNSP)
- Patient payment Collection rate
- Point of service (POS) and upfront collection rate
- Clean claims rate (CCR)
- Denied claims rate
- Gross collection rate
- Net collection rate
- Revenue realization rate (RRR)
- Streamline patient experience:
The satisfaction of customers is the foundation on which every business survives. Providing exceptional patient care fosters the patient-provider relationship, improves patient retention rates, and thus forms loyal customers. They are also more likely to recommend your practice to others, thus generating higher revenue through word-of-mouth referrals. You can increase customer satisfaction by:
- Efficient patient registration – Have a versatile patient appointment system in place with different options like online booking, phone-call booking or front desk booking so that patients are free to choose their preference. Send out notifications with automated reminders to notify patients head of appointments to reduce late arrivals, no-shows, or cancellations.
- Fill cancellations – Unfortunately, last-minute cancellations are unavoidable. Save time by sending an automated message in the event of cancellations to the rest of the waiting patients so that you don’t lose both your time and money.
- Online reviews – Encourage your patients to share positive reviews online so that your practice enjoys greater visibility and attracts new patients. Respond to any reviews, negative or positive, professionally and provide solutions.
- Automate patient verification and payment process:
Gone are the days when staff members were assigned the manual, repetitive task of jotting down every piece of information on paper. By automating the patient eligibility verification process, you reduce the risk of claim denials and human errors. Automation also ensures patients can enter their own information online ahead of treatment and schedule an appointment at their convenience, so your staff is free to focus on more critical matters.
Health plans require prior authorization, and it can be difficult to get these approvals on time. This could disrupt your schedule. The manual verification process is expensive, and you can reduce this cost by opting for electronic prior authorizations which will bring you valuable cost savings.
According to the Academy of Healthcare Revenue, your chance of collecting payments at the time of service is around 70%, but it lowers to 30% after the patient leaves the office.
Providers have a responsibility to be as transparent as possible about the costs with their patients and ease the financial process. You can simplify financial transactions by providing estimates before the actual service, offering different modes of online payments which facilitate timely payments. Proactive collection ensures upfront, regular cash flow and reduces outstanding balance thereby maximizing revenue.
- Improve medical coding:
Accurate medical coding is the cornerstone of healthcare revenue cycle management. Ensure your coding staff is trained and up to date with the latest coding guidelines and regulations set by the state and the insurance companies. Working with a medical coding company ensures accurate medical documentation, helps maintain assurance compliance, and improves medical billing.
Medical coding cannot be done efficiently without accurate, complete documentation practices. Implementing electronic health records (EHR) systems with integrated features like charting, medication management, billing and coding assistance aids in streamlining the documentation and coding process. Any wrong code or errors will disrupt your reimbursement flow.
- Modernize claim processing:
Claims scrubbing used to be a long and arduous process that had to be done manually. With the advent of modern claim scrubbing software, the process has become much simpler. You can use claim scrubbing software to verify the accuracy and rectify errors before submission to reduce denials. This technology-driven approach assures prompt payment, so there are no delayed or under payments left.
- Have a good claim management team:
A major cause of concern when it comes to administrative work is the pilling up of unpaid claims, claim rejections, claim denials and slow insurance verification process. However, effective claim management ensures that your practice is properly compensated for your medical services, procedures, equipment and care in a timely manner. Key steps in denial management include:
- Identify and examine the root cause of denials as the first step to get a clear picture of where the denials occur most frequently. Patient eligibility, coding errors, missing data, late submissions, outdated CPT OR ICD-10 codes, out-of-network care, and lack of prior authorizations are usually the top reasons for claim refusal.
- Categorize and sort denials based on the reason to understand the systematic issues for future preventions.
- After analyzing and categorizing the denials, you can correct and re-submit the claims for payment.
- Develop a tracking mechanism to regularly monitor and review the progress of resubmitted claims.
- Hire experts or train your staff with the information gathered to prevent the same denials from occurring.
- Collaborate with insurance providers:
Collaborating with insurance providers improves the quality of patient care and has a significant impact on your practice’s revenue. In a study conducted by the American Medical Association on a program that involved a health insurer working with providers to improve care for patients with chronic conditions, it was found that over a period of two years, there was 25% reduction in hospital admissions and 17% reduction in emergency room visits, which resulted in $30 million cost savings.
Another study held by the Journal of Managed Care & Specialty Pharmacy for medication therapy management services to patients concluded that collaboration between insurance providers and healthcare practices resulted in 4% increase in medicine adherence which led to a cost savings of $1,260 per patients per year.
- Diversify your services:
Expanding your services to include specialized treatments, wellness programs, and preventive health screenings will help open new avenues for revenue streams and offer a safety net to your current income. Increase your practice’s potential by tapping into new patient demographics and cater to a broader patient base by incorporating ancillary services that make sense as part of your practice.
- Leverage Telemedicine services:
Telemedicine service is the future in the healthcare industry and allows medical facilities to expand their reach beyond their immediate geographic location. When in-person consultation poses to be a limitation or a challenge, telehealth offers an alternative by being safely accessible and generates additional revenue. The rise of telemedicine is transforming the physician-patient relationship as it provides remote consultations, reduces cancellations or no-shows and minimizes travel costs for both providers and patients.
Telehealth has surged under COVID-19 and the size of the global virtual care market is expected to reach $285.7 billion by 2028. So, it is safe to assume that a practice without telemedicine service may fall behind.
- Utilize key statistics:
Constantly assessing your practice’s financial KPIs is essential to gain insights into the efficiency of your RCM. Use analytics tools to gauge areas for improvement, make data-driven decisions and maximize revenue potential. Important KPIs worth tracking include:
- Total reimbursement collected
- Net collections’ ratio
- Operating margin
- Average revenue per patient visit
- Patient acquisition cost
- First pass acceptance rate
- Denial rate
- Days in accounts receivable
Tracking your KPIs regularly and analyzing trends can help you see what’s working and not working.
Financial optimization in healthcare requires a multi-faceted approach that encompasses various aspects of patient engagement, upgrading technology, efficient coding, and revenue management. Constant regulatory changes to healthcare policies, coding guidelines and reimbursement models mean continuous updating to the same. Your practice’s administrative process can be eased by relying on third-party RCM experts. Outsourcing medical billing brings in a customized system fine-tuned to your needs, which streamlines your workflow and maximizes revenue generation.
Optimize your front-end and back-end processes and take control of your revenue cycle!