Chronic obstructive pulmonary disease (COPD) is an ongoing lung condition caused by damage to the lungs, according to the Mayo Clinic. COPD obstructs airflow and interferes with normal breathing. Emphysema and chronic bronchitis are the primary conditions that make up COPD, often occurring together. The American Lung Association estimates that COPD affects 11.7 million adults and accounts for hundreds of thousands of emergency department visits annually, costing the healthcare system tens of billions of dollars each year.
Accurately coding chronic respiratory conditions like COPD is challenging due to the complexity of the condition, overlapping symptoms, and the need for precise differentiation between chronic, acute, and exacerbated forms. ICD-10-CM guidelines require careful attention to Excludes1 and Excludes2 notes, combination coding, and specificity in documentation to ensure claims are correctly processed. Errors in coding can lead to denials, delayed reimbursements, and compliance risks. As a medical billing company handling a high volume of claims for this condition, we have in-depth expertise in the ICD-10 coding complexities related to COPD.
Need expert medical coding services for COPD treatment?
Causes and Symptoms
COPD includes a range of chronic, progressive, obstructive lung diseases usually caused by smoking and other environmental factors.
- Smoking — the primary cause of COPD
- Prolonged exposure to environmental irritants (toxic fumes, dust, air pollution, secondhand smoke, etc.)
- History of serious childhood respiratory infections such as pneumonia
- Gastroesophageal reflux disease (GERD) may cause or worsen COPD
- Genetics — deficiency of alpha-1 antitrypsin (AAT), a protein produced in the liver
Symptoms of COPD include chronic cough or cough with large amounts of mucus, shortness of breath that worsens with exertion, wheezing and tightness in the chest, fatigue, and low oxygen blood saturation. Exacerbations or symptom flare-ups can range from mild to life-threatening.
ICD-10 Codes for COPD
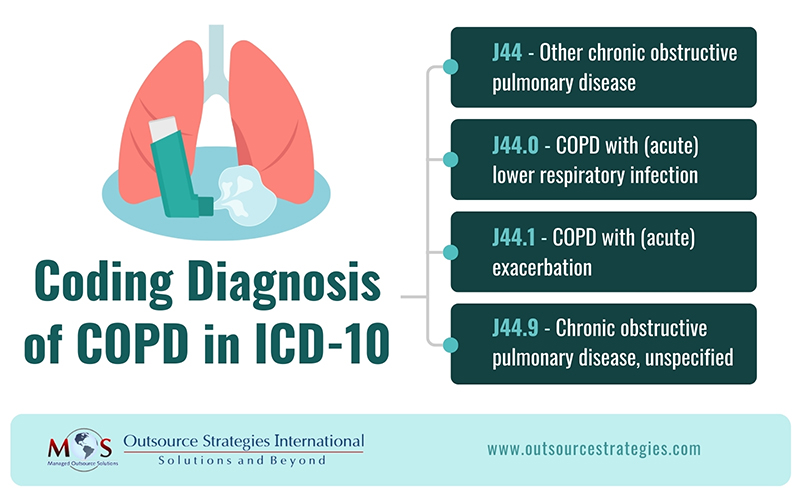
COPD is a general term that represents conditions such as emphysema, asthma, or chronic bronchitis, all of which cause airway obstruction, according to AHA’s ICD-10-CM and ICD-10-PCS Coding Handbook Revised 2024 Edition. COPD often results from underlying conditions such as chronic bronchitis or emphysema. In ICD-10, these conditions are classified to category J44, Other chronic obstructive pulmonary disease. A fourth character provides greater specificity to this code:
J44 Other chronic obstructive pulmonary disease – includes asthma with COPD, chronic asthmatic bronchitis, and chronic obstructive asthma, among other diagnoses
J44.0 COPD with (acute) lower respiratory infection – used to report cases where a patient with COPD develops an acute infection in the lower respiratory tract, such as bronchitis or pneumonia
J44.1 COPD with (acute) exacerbation – used when the patient experiences worsening COPD symptoms (e.g., increased dyspnea, wheezing) without an infection
J44.0 and J44.1 are assigned together when documentation shows a patient with an acute lower respiratory infection as well as an acute exacerbation.
J44.9 Chronic obstructive pulmonary disease, unspecified – used when the specific type of COPD is not known
ICD-10 Tips for Accurate COPD Claim Submission
- Scrutinize Provider Documentation
The details of the assigned code’s description must match the provider documentation of the diagnosis. Here’s an example from a Find-a-code article:
- Report J44.0 if the documentation shows a patient with COPD presents with an acute lower respiratory infection, such as acute bronchitis.
- If the patient presents with an acute exacerbation of their COPD and chronic bronchitis, then report J44.1 and a code for chronic bronchitis (J42)
- Do not Code Symptoms explained by a Confirmed Diagnosis
According to ICD-10-CM coding guidelines, symptoms should not be reported when they are attributed to a confirmed condition. If the documentation shows a patient who is a smoker with COPD and acute bronchitis, with symptoms of shortness of breath and cough, assign the following codes:
- J44.0 Chronic obstructive pulmonary disease with acute lower respiratory infection
- F17.210 Nicotine dependence, cigarettes, uncomplicated
Here, codes are not assigned for cough and shortness of breath since these symptoms are common to both COPD and acute bronchitis—both confirmed diagnoses.
- Know the Codes for Other Respiratory Illnesses
One challenge is to ensure accurate coding when patients present with COPD and another respiratory illness such as asthma, emphysema, or bronchiectasis. Pulmonology coders have to be knowledgeable about the codes and guidelines for these conditions to ensure accurate coding of chronic respiratory conditions.
- COPD with coexisting asthma COPD
COPD with unspecified asthma is included in category J44 and codes to J44.9. If the type of asthma is further specified, two codes are assigned: a code from category J44 for COPD; and a code from category J45 to report the type of asthma. Subcategories under J45 include:
- J45.2- Mild intermittent asthma
- J45.3- Mild persistent asthma
- J45.4- Moderate persistent asthma
- J45.5- Severe persistent asthma
- J45.9- Other and unspecified asthma
Fifth and sixth characters are added to indicate if the asthma is uncomplicated, with exacerbation or with status asthmaticus.
When the medical record documentation shows both acute exacerbation of asthma AND status asthmaticus, assets.humana.com clarifies that only the code for the more severe condition, status asthmaticus, should be assigned.
- COPD with acute exacerbation and acute bronchitis
Exacerbation of COPD is a periodic worsening, flare-up or decompensation of symptoms. An exacerbation means a worsening of the chronic condition, not the same as an infection, though infections can trigger a COPD exacerbation.
Code J44.1, COPD with acute exacerbation should be used when the documentation clearly states that the patient is experiencing a worsening of respiratory symptoms beyond normal day-to-day variation, requiring a change in therapy.
This code has an Excludes2 note stating code J44.0 is not part of the condition represented by code J44.1. This signifies that both codes can be assigned when the medical record shows both conditions are present.
COPD with acute bronchitis (an acute infection) is coded:
- J44.0 Chronic obstructive pulmonary disease with (acute) lower respiratory infection
- J20.9 Acute bronchitis, unspecified
- COPD with bronchiectasis
When COPD coexisting with bronchiectasis is documented, ICD-10 guidelines state that only a code from category J47 is assigned. Category J44 Excludes1 COPD with bronchiectasis and redirects the coder to category J47, bronchiectasis. Category J47 has multiple instructional notes and fourth characters to provide greater specificity.
- Emphysema
Emphysema documented with coexisting chronic bronchitis classifies to category J44. Emphysema without mention of chronic bronchitis classifies to category J43.
- Other Specified and Unspecified Codes
If documentation lacks the detail needed for a specific COPD code, use an unspecified code. However, if a specific type of COPD is documented but no exact ICD-10-CM code exists, report J44.89 (Other specified COPD). For example, J43.8 (Other specified emphysema) is a specified type—if the documentation doesn’t match this, use J44.89 instead.
- Follow Instructional Notations and Guidelines
Following instructional notations and guidelines like Excludes1, Excludes2, Code Also, and Use Additional is essential for accurate, complete coding and ensuring the highest level of specificity.
For example, J44 has an Excludes 1 note that prohibits reporting codes in that category with J43.9 Emphysema, unspecified. So if documentation indicates a patient with emphysema presents due to asthma and COPD, HCPCS Coding Clinic® (vol. 6, no. 1), instructs reporting J43.9 for the emphysema and a code from J45.- for the asthma. The reasoning is that emphysema is a more specific form of COPD, so you don’t need an additional code to represent unspecified COPD (aapc.com/blog).
To prevent COPD coding errors, it’s essential to pay attention to the notes in the ICD-10 Tabular List. With payers closely monitoring compliance with Excludes1 notes, adhering to these guidelines can help reduce claim denials.
Ensure Claim Accuracy: Partner with an Expert
Accurately coding COPD and related conditions requires a deep understanding of ICD-10 pulmonary disease coding guidelines, including Excludes1 and Excludes2 notes, combination coding, and specificity requirements. The complexities of distinguishing between acute exacerbations, infections, and overlapping respiratory conditions make pulmonology coding particularly challenging. Errors in reporting can lead to claim denials, revenue loss, and compliance risks.
By outsourcing medical billing and coding to experienced professionals, healthcare providers can ensure accuracy, reduce administrative burdens, and improve reimbursement outcomes. Expert coders carefully examine the physician documentation for COPD and stay up to date with the latest regulatory changes, ensuring accurate coding and claim submission, minimizing denials and optimizing revenue cycle efficiency. Experts ensure adherence to best practices for coding moderate to severe COPD, optimizing reimbursement and allowing providers to focus on delivering exceptional patient care.
Stay compliant with evolving coding guidelines!
Maximize reimbursement for pulmonology claims!