Gingivitis is a common form of gum disease that causes swelling, redness and irritation of gingiva – the part of your gum around the base of your teeth. One of the most common causes of gingivitis is poor oral hygiene. Poor oral health habits often leads to build-up of plaque (a naturally-occurring sticky film containing bacteria) on the surface of teeth that causes inflammation of the surrounding gum tissue. Plaque produces toxins that irritate the gums causing severe inflammation and making them red or puffy eventually causing bleeding when a person brushes his/her teeth. As plaque advances, it hardens and becomes tartar. Plaque can develop into an infection when it extends below the gum line. If left untreated, this condition can progress to gum disease that spreads to underlying tissue and bone (periodontitis), a much more serious condition that can lead to tooth loss. In addition, chronic gingiva inflammation has been thought to have direct association with some systemic diseases such as respiratory disease, diabetes, coronary artery disease, stroke and rheumatoid arthritis. Early identification of symptoms and risk factors that directly contribute to this gum disease can help prevent the condition in the long run. As dental medical billing and coding involves several complexities, physicians must have knowledgeable teams and business systems in place to correctly document the procedures performed. Medical billing outsourcing is an option worth considering as this can help physicians ensure accurate and timely claim filing and reimbursement.
According to the American Dental Association, gingivitis and periodontitis are the major causes of tooth loss in adults. It is estimated that this gum condition occurs in 3 out of 4 Americans during their lifetime. However, with early and proper dental care, many of its symptoms can be easily reversed. Good oral health habits, such as brushing at least twice a day, flossing daily and getting regular dental checkups, can help prevent and reverse the symptoms of gingivitis.
Classic Symptoms of Gingivitis
Generally, many people aren’t aware that they have gingivitis. In most cases, this gum disease occurs without any specific symptoms. In mild cases of gingivitis, there may be no discomfort or noticeable symptoms. Common signs and symptoms include –
- Bright red or purple gums
- Tender gums that may be painful to the touch
- Receding and soft gums
- Pus between teeth and gums
- Inflammation or swollen gums
- Halitosis or bad breath
- Bleeding from the gums when brushing or flossing
- A change in how your teeth fit together when you bite (malocclusion)
Reports from the Centers for Disease Control and Prevention and the National Institute of Dental and Craniofacial Research suggest that gingivitis is associated with an increased risk of diabetes, heart disease, stroke, and lung disease. It also increases the risk of a woman giving birth to a premature or low birth weight infant.
Several factors that can increase your risk of gingivitis include – smoking or chewing tobacco, dry mouth, crooked teeth, dental restorations (that don’t fit properly), use of certain medications (oral contraceptives, steroids, anticonvulsants, calcium channel blockers, and chemotherapy) and hormonal changes.
How Is Gingivitis Diagnosed and Treated?
Initial diagnosis of gingivitis may begin with a detailed review of dental and medical history and conditions that may contribute to your symptoms. The dentist or periodontist would conduct a detailed examination of your teeth, gums, mouth and tongue for signs of plaque and inflammation. They will probe your gums with a small ruler and measure any pockets around your teeth. In addition, your dentist may also order imaging tests like X-rays to check for bone loss.
Regular and timely treatment help to reverse the symptoms of this gum condition and prevent it from progressing to a more serious gum disease and tooth loss. Treatment modalities for this condition include – deep cleaning your teeth, antibiotic medications and surgery.
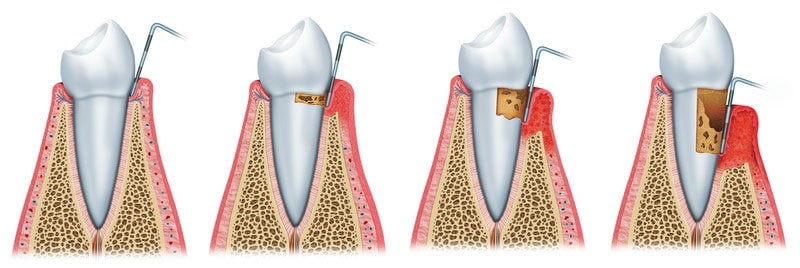
Professional dental cleaning removes all traces of plaque, tartar and bacterial products – a procedure called scaling and root planning. Scaling removes tartar and bacteria from tooth surfaces. Root planning on the other hand, removes the bacterial products produced by inflammation, softens the root surfaces and prevents further buildup of tartar and bacteria. Root planning procedure may be performed using laser technique or an ultrasonic device. Lasers may remove tartar with less pain and bleeding than scaling and root planning. Dental restoration may be done to fix misaligned teeth or poorly fitting crowns, or bridges that irritate your gums and make it harder to remove plaque during daily oral care. Medications include – Antiseptic mouthwash, Oral antibiotics, Doxycycline and timed-release antiseptic chips containing chlorhexidine can be inserted into pockets after root planing.
Surgery will be considered as a last resort if the above non-surgical treatment methods are not effective. Surgical techniques include – flap surgery (a procedure where the gums are lifted back while plaque and tartar is removed from deeper pockets), soft tissue grafts (can be used when teeth and jaw are too damaged to heal), and bone grafting.
Dental medical coding involves using the specific ICD-10 diagnosis codes to report various dental conditions such as gingivitis on the medical claims providers submit to health insurers. Dentists or periodontists who perform dental surgery need to submit accurate documentation that meets payer guidelines. Therefore, in addition to medical billing and coding services, dental insurance verification and pre-authorization services are crucial to verify patient’s coverage.
ICD-10 Codes to Use
- K05 – Gingivitis and periodontal diseases
- K05.0 – Acute gingivitis
- K05.00 – Acute gingivitis, plaque induced
- K05.01 – Acute gingivitis, non-plaque induced
- K05.1 – Chronic gingivitis
- K05.10 – Chronic gingivitis, plaque induced
- K05.11 – Chronic gingivitis, non-plaque induced
Preventing Gingivitis
Practicing proper and consistent oral hygiene is one of the primary steps to prevent the occurrence of gingivitis. Make a habit to brush your teeth twice daily with fluoride toothpaste. Floss your teeth every day. Eat a balanced diet and get regular professional dental cleanings on a schedule recommended by your dentist. Other prevention strategies include – cut back on smoking or chewing tobacco, use a mouth rinse to help reduce plaque, supplement brushing and flossing with an interdental cleaner, (such as a dental pick, interdental brush or dental stick) specially designed to clean between your teeth.
Medical coding for gum disorders can be a challenging process. For accurate and timely medical billing and claims submission, healthcare practices can outsource their medical coding tasks to a medical billing company that provides the services of AAPC-certified coding specialists.