Verification of patient benefits is a key aspect of the medical billing process and is performed to confirm an individual’s insurance eligibility and coverage. Healthcare professionals, insurance verification services, and insurance companies must ensure they are compliant with laws, regulations, and ethical standards. Let’s take a look at the key legal and ethical standards for insurance verification in practices and what compliance implies.


Ensure compliance and streamline your processes with our cutting-edge insurance verification services!
Legal and Ethical Aspects of Patient Eligibility Verification
The primary legal and ethical considerations impacting insurance verification are:
Patient Privacy
Insurance verification involves the collection and exchange of sensitive patient information between healthcare providers and insurance companies. It is crucial to maintain strict confidentiality during this process. Only authorized individuals directly involved in insurance verification should have access to patient information, and proper security measures should be in place to protect against unauthorized access or breaches
Compliance with legal regulations helps protect the rights and privacy of patients. It means that patient information must be securely handled, stored, and only accessed by authorized personnel involved in the verification process.
Healthcare providers and insurance companies must comply with privacy laws, such as the Health Insurance Portability and Accountability Act (HIPAA), the Fair Credit Reporting Act (FCRA), anti-discrimination laws, and state insurance laws.
- HIPAA requires covered entities and their business associates, such as insurance verification companies, implement appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information (PHI).
- When credit reports are used in the insurance verification process, compliance with the FCRA ensures consumers’ privacy remains intact and that credit information is reported fairly and accurately.
- Insurance verification must also adhere to non-discrimination principles, refraining from bias based on protected characteristics like race, gender, age, disability, or national origin.
- Compliance with state-specific insurance laws means adherence to state-mandated insurance coverage, verification procedures, and permissible handling of personal information.
- Insurance verification may involve agreements with a third-party vendor such as insurance verification services or with insurance companies. Ensure compliance with contractual obligations and terms, including data security and confidentiality clauses.
Staying up-to-date with applicable laws and regulations is critical to ensure legal and ethical compliance.
Informed Consent
When it comes to insurance verification, patients must provide informed consent for their insurance to be verified after being provided with comprehensive and clear information about what the verification involves. Obtaining informed consent in insurance verification is a legal requirement as well as an ethical obligation to respect individuals’ rights and privacy. Individuals should be informed about the purpose of insurance verification, the types of information that will be collected, and how that information will be used by the healthcare provider and insurance company. Patients have the right to refuse or limit the use of their personal information for purposes other than insurance verification.
Data Accuracy
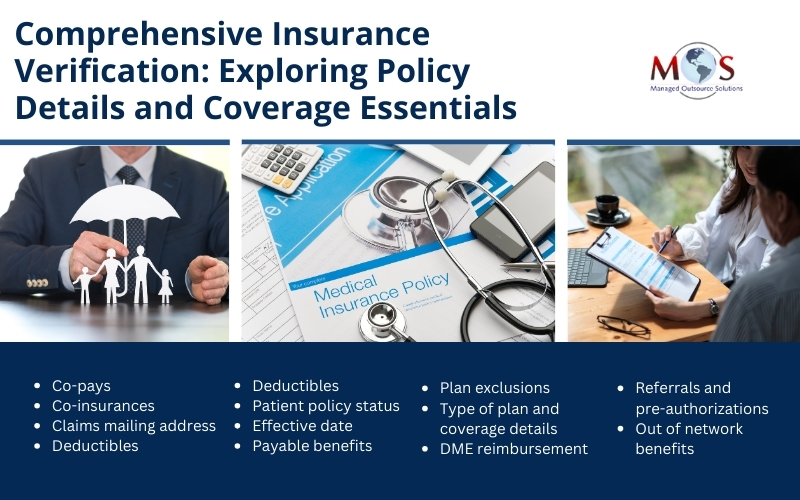
Insurance verification requires accurate and up-to-date information to determine coverage eligibility. In addition to verifying patient demographics, insurance verification involves checking the following insurance policy details and coverage information.
Healthcare providers and insurance companies have a legal and ethical obligation to ensure that the data collected during the verification process is accurate and reliable. Misrepresentation or manipulation of data can lead to ethical concerns and potential harm to individuals.
Transparency and Communication
Open and transparent communication with patients regarding insurance verification is important. Patients should be informed about the purpose, process, and potential outcomes of insurance verification.
For example, when a patient seeks medical services at a practice, the front desk should provide them with a clear explanation of the insurance verification process and how it can streamline their experience and minimize any financial surprises. The staff should tell the patient about the specific details they will need to verify and also inform them about any issues that arise during the verification, such as coverage discrepancies, authorization requirements, or any potential out-of-pocket costs. After the verification is complete, the staff should discuss the results with the patient and make sure they are aware of what their insurance will cover, co-payments, and deductible status. Clear and easy-to-understand explanations should be provided to address any questions or concerns that patients may have.
Documentation
Healthcare providers and insurance companies should maintain proper records of insurance verifications. These records may be required for auditing, compliance, or dispute resolution purposes. Following appropriate record retention policies and procedures is crucial to ensure the integrity and accessibility of these records.

Curious to learn more?
Check out our detailed exploration on compliance and quality assurance: Compliance and Quality Assurance in Insurance Verification
How Outsourcing Insurance Verification can Help
Navigating the legal aspects of insurance verification is easier when the process is handled by experienced professionals. By working with a reliable insurance verification company, practices can establish a framework to stay in compliance with legal and regulatory requirements as they evolve. Experts will handle the process to ensure protection of patient privacy, maintain data accuracy, preserve confidentiality, prevent discrimination, and meet applicable regulations.


Contact us today for a tailored insurance verification solution that meets your specific needs!