Irritable Bowel Syndrome (IBS) is a gastrointestinal disorder that affects millions of individuals worldwide. For healthcare professionals, accurately coding IBS-related diagnoses and treatments is essential for effective patient care, billing accuracy, and compliance with healthcare regulations. Accurate coding for IBS is vital not only for billing accuracy but also for maintaining compliance with evolving healthcare regulations. Gastroenterologists and other specialists can turn to professional medical billing outsourcing companies to ensure precise reporting of IBS diagnoses and screenings.
Remaining current with the most recent coding guidelines and updates is essential to uphold compliance and optimize reimbursement. Coding for IBS entails the selection of suitable ICD-10 diagnosis codes and CPT (Current Procedural Terminology) codes.
Challenges Associated With Medical Coding for IBS
The key challenges associated with medical coding for IBS are:
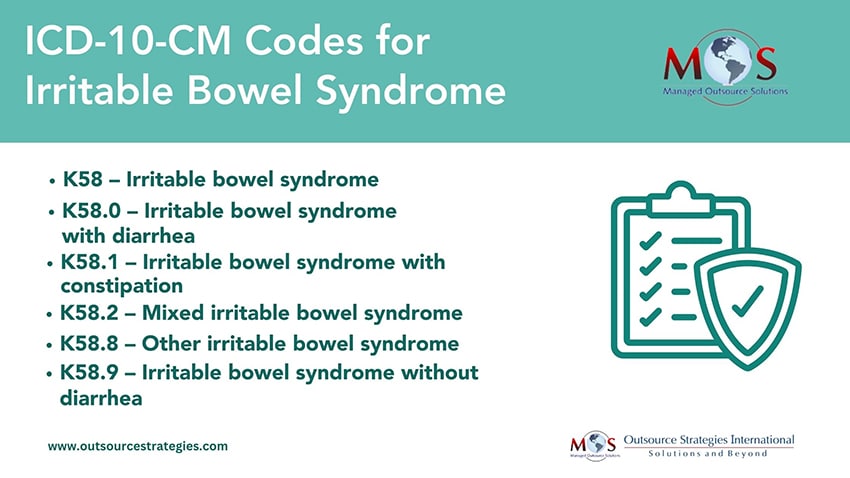
- Specificity in ICD-10 diagnosis coding: IBS is often diagnosed based on clinical criteria, as there is no specific test to confirm the condition. This can lead to coding challenges when trying to establish a definitive diagnosis code. Coders must rely on detailed documentation from healthcare providers, including symptoms, duration, and the absence of alarm features, to assign the most appropriate diagnosis code. It’s crucial to code to the highest level of specificity, such as differentiating between IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), and mixed-type IBS (IBS-M).
- Frequent updates to coding guidelines: Coding guidelines and conventions can change over time, affecting how IBS codes are assigned. Staying updated with the latest changes can be challenging for coders. Regularly refer to coding resources, attend coding seminars or webinars, and collaborate with coding experts to ensure that you are aware of any updates or revisions to coding guidelines related to IBS.
- Co-morbid conditions: Patients with IBS often have co-morbid conditions, such as anxiety or depression, which may require additional codes to reflect the complete clinical picture. Coders should review the patient’s medical records thoroughly to identify and accurately code all co-morbid conditions. Proper documentation from healthcare providers is crucial to support these additional codes.
- Documentation and specificity: Incomplete or vague documentation can make it difficult to assign precise codes for IBS-related services. Coders should work closely with healthcare providers to ensure that documentation is detailed and specific. Encourage providers to include information on symptom severity, duration, and any diagnostic criteria used.
- Understanding insurance coverage: Different insurance companies may have varying policies regarding IBS-related services, treatments, and coding requirements. Familiarize yourself with the policies of the major insurance providers and regularly communicate with the billing department to ensure proper coding and billing compliance.
Coding for IBS presents certain challenges due to its clinical nature and evolving coding guidelines. Attention to detail, continuous learning, and collaboration between coders and healthcare providers is crucial for accurate coding to support reimbursement, maintain high standards of patient care, and ensure compliance with healthcare regulations.
Optimize your practice’s financial health with our proven gastroenterology billing services!





