Medical billing in orthopedic practices involves complex surgical coding, bundled service rules, and high-dollar healthcare claims that receive intense payer scrutiny. These complexities make the process vulnerable to reimbursement delays, underpayment, and outright denials that significantly impact cash flow. From payer-specific modifier rules to intricate pre-authorization requirements, each step carries potential for costly errors.
That’s where effective denial management in orthopedic billing becomes not just a corrective measure, but a proactive strategy to reduce denied and rejected claims. By identifying common trigger points such as inaccurate coding or missed filing deadlines, denial management allows healthcare providers to take targeted steps to minimize revenue leakage. Providers can partner with denial management services specializing in orthopedic billing to efficiently address claim rejections, recover lost revenue, and safeguard the practice’s bottom line.
Understanding the Unique Challenges in Orthopedic Denial Management
Unlike other specialties, orthopedic billing presents distinct challenges that make denial management demanding for practices.
- High-value claims: In orthopedic care, both surgical procedures (such as joint replacements and fracture care) and diagnostic imaging (such as MRI or CT scans) generate substantial reimbursement amounts. The high costs of these services attract greater scrutiny from payers, resulting in higher denial rates.
- Diverse payer types: Orthopedic practices must navigate multiple payer types, including Medicare, commercial insurers, and workers’ compensation programs. Each payer comes with unique coverage policies, prior authorization requirements, and reimbursement rates, complicating the orthopedic billing process.
- Complex documentation requirements: Orthopedic procedures require detailed documentation including comprehensive operative notes, imaging reports and specific diagnosis codes to substantiate medical necessity. Insufficient documentation can lead to payment delays or payer claim denials.
- Frequent regulatory updates: The healthcare industry is subject to frequent regulatory changes, including updates to coding systems, payer policies, and billing standards. Orthopedic providers must stay informed about these changes to avoid penalties or rejections caused by outdated practices and ensure compliance.
- Administrative workload: The combination of high-value claims, diverse payers, and complex regulations increases administrative workload. Healthcare providers must carefully track submissions, manage appeals, and ensure compliance to minimize errors and financial risk.
Even a small oversight in any of these processes can result in denials that delays payments for weeks, or sometimes months. Without a structured process for tracking, analyzing, and resolving denials, practices face repeated billing errors, high denial rates, and ongoing revenue loss.
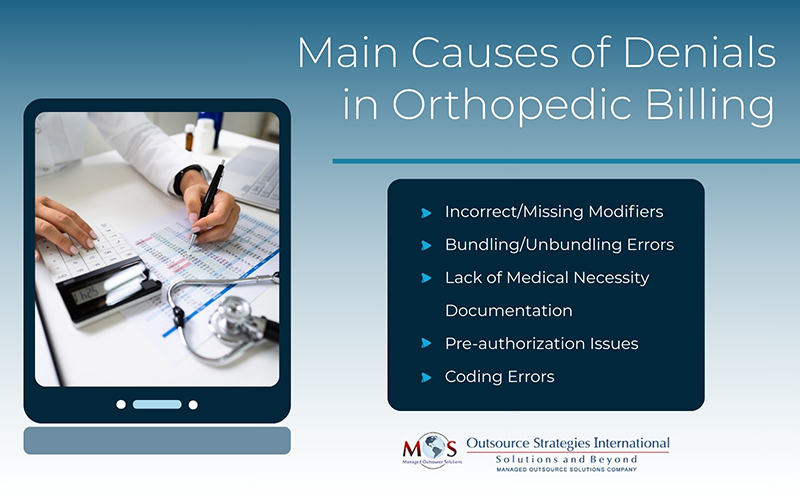
Common Causes of Claim Denials in Orthopedic Practices
Denials in orthopedic billing stem from multiple issues that can occur at different stages of the billing process. Coding inaccuracy, documentation gaps, or even a simple patient information mistake can collectively contribute to reimbursement delays. Understanding the most frequent reasons for denials can help healthcare providers take proactive steps to prevent rejections and protect revenue cycles.
- Incorrect/ missing modifiers: Orthopedic billing relies heavily on modifiers such as -LT, -RT, -50, – 25, and -59 to specify laterality, multiple procedures, or distinct services. Common errors include applying the wrong modifier combination or omitting the correct modifier entirely. Both scenarios can lead to claim disputes or reduced payments.
- Incorrect bundling or unbundling of services: Some orthopedic services are bundled together under payer rules, meaning they should be billed as a single line item. Unbundling these services without justification, or failing to bundle them when required, can cause denials and compliance issues.
- Lack of medical necessity documentation: Payers require detailed records showing why a specific procedure or test was needed. For example, joint replacements may require proof of tried and failed conservative treatments before approval. Missing or incomplete documentation is a common reason for denials in orthopedic practices.
- Pre-authorization errors: Surgeries, MRIs, and certain vaccines almost always require pre-authorization to be obtained before the orthopedic procedure. Missing, incorrect, failed, or expired authorizations can result in immediate claim denials.
- Medical coding inaccuracies: Given the complexity of orthopedic procedures, coding errors are frequent. These include the use of outdated/deleted CPT codes, missing specificity in diagnosis codes, or mismatching diagnosis and procedure codes.
Recognizing these recurring causes is the first step toward resolving denial issues at the beginning itself, preventing future rejections, and optimizing denial management strategies.
Effective Denial Management Strategies for Orthopedic Clinics
Creating a solid denial management process in orthopedic billing requires a structured, step-by-step approach that addresses problems at their root. The goal is not only to fix denials after they occur, but also to prevent them from happening in the first place. Healthcare providers can implement the following strategies to build an optimized denial management system that protects revenue and reduces administrative work:
- Denial trend analysis: Maintain a denial tracking system to categorize and analyze denied claims based on payer reason codes. Examine historical denial patterns to identify recurring coding errors, authorization issues, documentation gaps, and payer-specific challenges. These data-driven insights enable targeted corrective actions, reduce repeat errors, and improve first-pass claim acceptance rates.
- Streamlined appeal processes: When denials do occur, having a well-defined appeal process to resubmit, follow-up, and review the outcomes increases the likelihood of claim reversals. Practices can establish structured appeal management with standardized templates, necessary supporting documentation and advanced denial management software to expedite the resolution process.
- Regular claim audits: Periodically reviewing submitted claims helps providers identify recurring errors in surgical procedure coding, documentation gaps, or payer requirements. Early detection of these errors can prevent denials before they occur and improve overall claim accuracy.
- Staff training: Provide employee training and education by investing in regular certification programs, workshops, and compliance training. Thus, you can ensure they stay up-to-date on the latest coding and billing practices. Well-trained staff make sure that claims are submitted correctly the first time, minimizing chances of rejections.
- Leverage advanced technology: Utilizing automated denial management tools, intelligent EHR systems, and advanced analytics tools can significantly reduce manual efforts, human errors, and enhance claim accuracy rate.
Implementing these proven strategies will enable orthopedic practices to optimize billing operations, stay ahead of denials, and improve revenue cycle without compromising on patient care.
How Proactive Denial Management Helps Orthopedic Practices
Proactive denial management is instrumental in identifying denial triggers, implementing preventive measures, and enhancing approval rates for orthopedic claims. This forward-looking approach turns the exhausting cycle of appeals into a streamlined process of accuracy, compliance, and financial stability.
- Improved cash flow: Timely claim settlements ensure steady and reliable cash flow, allowing for better financial planning and investment in patient care resources for orthopedic practices.
- Enhanced first-pass claim acceptance: Claims are more likely to be approved on the first submission as they are supported by proper documentation, accurate coding, and verified patient eligibility and pre-authorizations.
- Reduced administrative burden: Proactive measures, including trend analysis, staff training, and automated workflows minimize the administrative burden of repetitive claim corrections and follow-ups, allowing you to better focus on patient care.
- Data-driven decision-making: Denial tracking and analytics give providers actionable insights to identify trends, analyze root cause, and implement targeted strategies for correction, prevention, and long-term improvement in claim outcomes.
- Strengthened compliance: A proactive approach ensures that coding, documentation, and billing practices remain up-to-date with regulatory and payer requirements, reducing the risk of audits, penalties, or rejections.
By implementing proactive denial management, orthopedic practices can not only protect revenue but also create a more efficient and compliant billing system that supports long-term financial health.
Optimize Denial Management with Outsourcing
Optimized denial management is essential for healthcare providers to maximize reimbursements, enhance operational efficiency, and maintain long-term financial stability. Orthopedic practices can partner with specialized orthopedics medical billing services to leverage expertise, advanced technology, and dedicated resources that handle denials more efficiently compared to in-house systems. This approach reduces administrative burden, accelerates reimbursements, and allows the in-house team to focus on patient care while ensuring that all claims are tracked, analyzed, and appealed promptly.
Get paid faster and more accurately with expert orthopedic billing support!




