In 2019, medical billing companies will help providers bill Medicare for Remote Patient Monitoring (RPM) with three new CPT codes. The American Medical Association (AMA) points out that Medicare’s new RPM codes recognize physicians’ increasing use of digital technologies to connect with patients. RPM services can be provided wherever patient is located, including at the patient’s home.
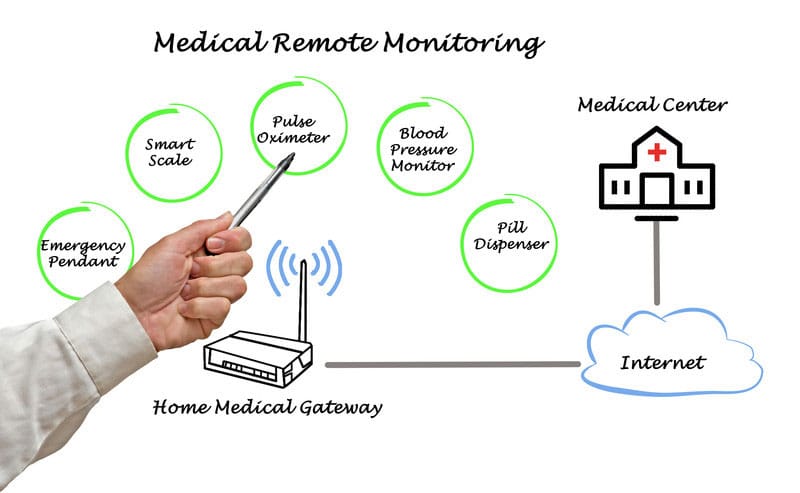
The term “remote patient monitoring,” refers to the use of digital technologies to collect medical and other types of health data from an individual in a location outside of conventional clinical settings and electronically transmit that information securely to a healthcare provider in a different location for assessment and recommendation. Similar to chronic care management (CCM), RPM is a type of telehealth delivery system that can improve health outcomes and reduce the cost of care.
New Separately-reimbursable RPM Codes in 2019
Using digital technology helps healthcare providers to connect with their patients more effectively and efficiently at home and collect data for care management and coordination. The three new codes to report RPM services in 2019 are:
- 99453 Remote monitoring of physiologic parameter(s), (for example, weight, blood pressure, pulse oximetry, respiratory flow rate) initial; setup and patient education on equipment use.
- 99454 Device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days.
- 99457 Remote physiologic monitoring treatment management services, 20 minutes or more of clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/caregiver during the month.
In addition to these three codes, two new interprofessional internet consultation codes, 99451 and 99452, have been created to reflect the increasing importance of using non-verbal communication technology to coordinate patient care between a consulting physician and treating physician.
- 99451 Interprofessional telephone/internet/electronic health record assessment and management service provided by a consultative physician, including a written report to the patient’s treating/requesting physician or other qualified health care professional, 5 minutes or more of medical consultative time.
- 99452 Interprofessional telephone/internet/electronic health record referral service(s) provided by a treating/requesting physician or other qualified health care professional, 30 minutes.
CPT Code 99091 – Medicare’s Current Code for RPM
Even before the introduction of these codes, Medicare covered RPM services billed under CPT code 99091. This code was created in 2002 to describe an interaction whereby patients use a home monitoring device (at that point in time, a glucose monitor) to collect their health information and transmit it to their doctor. However, for years, CMS bundled 99091 with other management services codes and it was not separately reimbursable as a standalone service.
RPM services became separately reimbursable under the 2018 Physician Fee Schedule. CPT Code 99091 was “unbundled”, allowing practitioners to seek separate Medicare reimbursement for RPM services. The 2018 Medicare Physician Fee Schedule Final Rule 2 defines code 99091 as “Collection and interpretation of physiologic data (e.g., ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient and/or caregiver to the physician or other qualified health care professional, qualified by education, training, licensure/regulation (when applicable) requiring a minimum of 30 minutes of time.” CMS also decided to allow practitioners to use RPM to improve their Merit-based Incentive Payment System (MIPS) score.
The following requirements need to be met to bill Medicare for RPM services under CPT 99091:
- The patients should give the practitioner consent for RPM services and this should be documented it in the patient’s medical record.
- For new patients or patients not seen by the practitioner within one year, RPM services must be initiated during an initial face-to-face visit with the practitioner, such as a Preventive Physical Exam or an exam included in Transitional Care Management.
- CPT 99091 should be reported no more than once in a 30-day period per patient. The service must include the time that the physician or other qualified health care professional spent with data accession, review and interpretation, modification of care plan as necessary (including communication to patient and/or caregiver), and associated documentation.
- CPT 99091 can be billed once per patient during the same service period as chronic care management (CCM) services (CPT codes 99487, 99489, and 99490), TCM services (CPT codes 99495 and 99496), and behavioral health integration services (CPT codes 99492, 99493, 99494, and 99484).
- Since Medicare does not consider RPM services as telehealth services, the patient can be at his/her home, and need not be in a rural area or qualifying originating site.
Implementing RPM Services
The AMA CPT Editorial Panel produced the new RPM codes to reflect the coding demands of the modern health care system and digital medicine. Inputs from practicing physicians, medical specialty societies and the health care community at large were taken into consideration. According to an article published by Telehealth and Medicine Today, practitioners implementing the new codes need to be vigilant about any HIPAA privacy and security vulnerabilities related to the use of new digital RPM technologies. They should also get their arrangements with technology vendors evaluated by a healthcare attorney for any potential AntiKickback and/or Stark Law implications. Outsourcing medical billing services can help healthcare providers report the new codes correctly to be reimbursed appropriately for their services.