Managing medical billing can pose significant challenges. Regardless of the size of a healthcare practice, billing and claims processing involves substantial costs. Secure and compliant medical billing outsourcing can ensure efficient revenue cycle management while lowering overhead costs.
Let’s explore the many ways outsourced medical billing services optimize workflow and reduce costs.
Let’s explore the many ways medical billing services optimize cost efficiency.

How Outsourcing Medical Billing reduces Overhead Costs
Did you know that each year, physicians in the United States lose approximately $125 billion in potential revenue as a result of poor billing and coding practices? The Healthcare Financial Management Association (HFMA) reported that lost charges, partly due to insufficient clinical documentation and inaccurate coding, cause hospitals to lose 3-5% of their revenue each year.
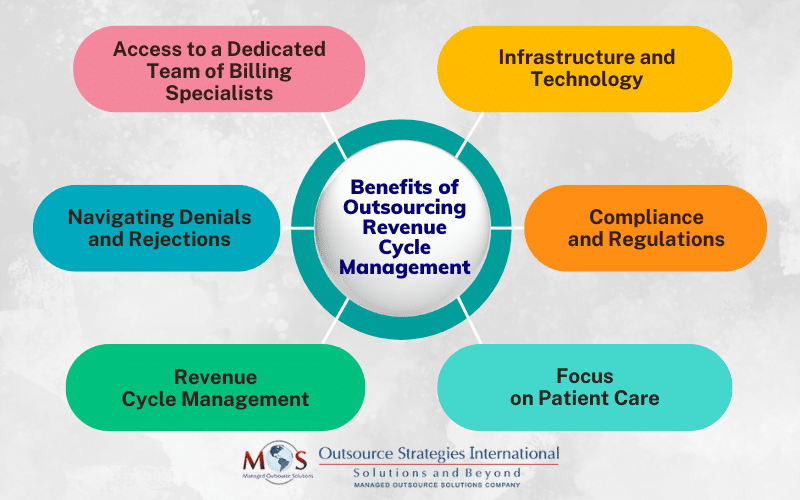
Outsourcing revenue cycle management, including medical billing, saves your practice money in many ways:
Infrastructure and Technology
Maintaining an in-house billing team necessitates various accommodations, such as office space, equipment purchases and maintenance, HR resources, and office supplies. Each of these accommodations incurs expenses, with rental fees and supply prices subject to unpredictable fluctuations. A comprehensive medical billing system requires careful consideration of these costs to ensure efficient operations.
Specialized IT infrastructure is essential to handle the intricacies and complexities of coding, claim generation, and submission, as well as facilitate seamless integration with insurance providers and other relevant parties. Medical billing software systems need to be regularly updated and maintained, which involves additional costs. In addition to software, specific hardware components such as servers, computers, and networking are needed to ensures the smooth flow of information, safeguard sensitive patient data, and support the efficiency of the billing process. Leveraging professional billing services gives your practice access to these specialized tools and robust IT infrastructure, eliminating the need to invest in and maintain them. This can be especially beneficial for small practices or those with limited resources.
Access to a Dedicated Team of Billing Specialists
Medical billing involve tasks such as insurance verification, coding diagnoses and procedures, preparing and submitting claims, and accounts receivable (AR) follow-up. Employing and maintaining an in-house team specialized in these areas can be costly, including expenses on salaries, health insurance, and other full-time benefits. In fact, the nationwide issue of medical billing and coding staffing shortages, resulting in a supply and demand issue, has also resulted in the push for higher wages. According to the American Medical Association (AMA), studies show that there’s a 30% shortage in medical coders.
“It’s not necessarily a significant turnover issue as much as it is growth, as we need additional coders to support how much we have grown over the last few years,” said Rhonda Hale, vice president of finance for Baptist Health Medical Group.
With changing regulations, medical coders and billers also need to stay up to date with continual training. Since a medical billing company provides this training for its own staff, you don’t have to worry about this aspect. Outsourcing saves money on staffing while giving your practice access to a team of skilled professionals who are knowledgeable about the latest billing and coding guidelines.
Navigating Denial Management
Medical claims can be denied or rejected for various reasons, such as incomplete or inaccurate information. Handling claim rejections and resubmissions can be time-consuming and resource-intensive, leading to increased costs. By outsourcing, you are ensured of a dedicated team with more time to follow up on claims and ensure revenue is coming in. A dedicated team can help catch trends in denials and help improve clean billing to increase reimbursement timeframes. They also verify patient insurance benefits before services are provided, which minimizes the risk of denials due to eligibility issues. Having experts handle medical insurance eligibility checks can ensure that you, accurately bill for services that are covered by the patient’s insurance plan. This minimizes the risk of underbilling or overbilling, leading to more accurate revenue capture.
Compliance and Regulations
Complex and ever-changing regulations such as the HIPAA (Health Insurance Portability and Accountability Act), the Affordable Care Act, ICD-10 coding, and the shift towards value-based payment models add to the challenges of healthcare billing. These developments have a direct influence on crucial aspects such as medical necessity determinations, precise clinical documentation, accurate coding, and effective charge capture processes. Failure to adapt to these changes may result in billing errors and delays in reimbursement. To maintain standards and gain a strategic edge in light of the current emphasis on coding and documentation guidelines requires investing in training, audits, and implementing security measures, which adds to the overall cost. Providers can reduce billing errors with third-party billing services that ensure accurate coding, timely submissions, and strict compliance with industry standards.
Revenue Cycle Management
In addition to medical billing, the revenue cycle includes activities like patient registration, insurance verification, claims processing, payment posting, and collections. Insurance verification can be difficult due to factors like the need to gather accurate and up to date patient data, frequent changes in insurance information, complex insurance policies, and varying coverage plans. Each step in the revenue cycle requires dedicated resources and expertise, involving associated costs. Not verifying patient eligibility before services are provided can lead to denials, affecting a practice’s finances.
Outsourcing billing to specialized third-party companies can reduce these expenses and improve claim turnaround time. By leveraging the expertise and resources of a professional company, you can streamline the process and benefit from the experience and knowledge of billing experts. This can result in significant cost savings and improved RCM. Outsourcing medical billing also plays a key role in healthcare cost reduction by minimizing administrative expenses and improving claim processing efficiency.
Focus on Patient Care
Building stronger doctor-patient relationships, providing thorough examinations, and addressing patient concerns become easier when you can concentrate on delivering quality care without being overwhelmed by billing-related responsibilities.
“Many clients that reach out to us are employees feeling extreme burn out due to juggling too many additional office tasks. When their actual job should be solely/mainly patient care, unfortunately, tasks such as preauth and verifying insurance often fall on their shoulders due to the staffing shortages or lack of experienced additional staff available to assist. Outsourcing those tasks makes for a less burdened/stressed out in-house staff. Happier employees, better patient care”, says Natalie Tornese CPC, OSI’s Director of Revenue Cycle Management, Healthcare Division.
Outsource Billing: Stay Updated and Save Money
As the medical billing landscape continually evolves, fresh challenges arise. Successfully navigating these emerging obstacles and improving cash flow requires staying abreast of industry trends, regulatory shifts, and technological advancements. By choosing the right medical billing partner, you can reduce costs and focus on what you do best – patient care.


Learn how our expert medical billing and coding services can save you time and money!
Call (800) 670-2809 Today!