The Affordable Care Act (ACA) requires health benefit plans that started on or after September 23, 2010 to provide coverage for colorectal cancer screening tests. For those plans that started before September 23, 2010, the rules about insurance coverage are determined by state laws that vary, and other federal laws. For all new beneficiaries, Medicare covers an initial preventive physical exam that occurs within one year of enrolling in the same. Under Medicaid programs, states are authorized to cover colorectal cancer screening. The coverage rules for screening varies by state and will differ in accordance with the specific type of Medicaid managed care plan a person is enrolled in.
Oncologists providing various treatment modalities should have up-to-date knowledge about the latest coding changes for the colon cancer screening services provided. Oncology billing and coding can be complex and a high level of knowledge and experience regarding appropriate coding, modifiers and payer-specific medical billing are vital for correct and on-time reimbursement.
The ICD codes for colorectal cancer include:
ICD-9 Codes
- V10.0 – Personal history of malignant neoplasm of large intestine (high risk screening code)
- V10.06 – Personal history of malignant neoplasm of rectum, rectosigmoid junction, and anus (high risk screening code)
- V12.72 – Personal history of adenomatous colonic polyps (high risk screening code)
- V16.0 – Family history of malignant neoplasm of gastrointestinal tract (first degree relative-sibling, parent, child) (high risk screening code)
- V18.51 – Family history, adenomatous colonic polyps (high risk screening code)
- V76.41 – Special screening for malignant neoplasms of rectum
- V76.51 – Special screening for malignant neoplasms of colon
- V84.09 – Genetic susceptibility to other malignant neoplasm (not covered by all payers)
ICD-10 Codes
- Z12.11 – Encounter for screening for malignant neoplasm of colon
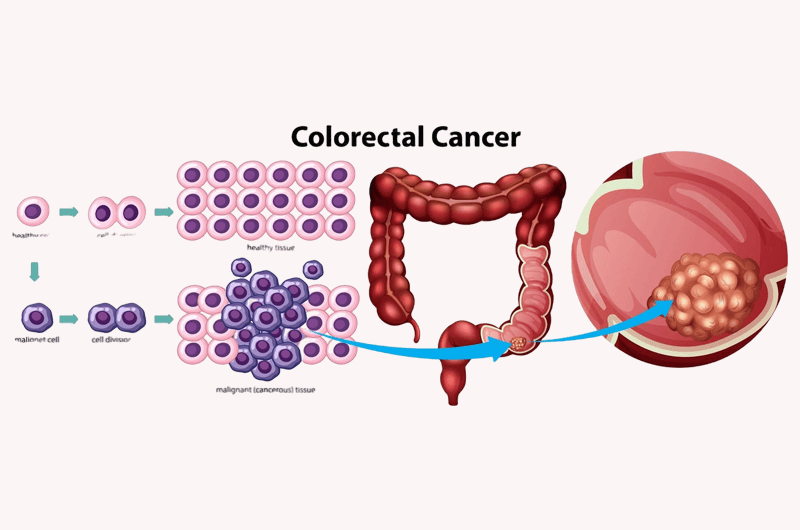
Colorectal cancer (CRC) is the third most commonly diagnosed cancer in the United States and the third leading cause of death among Americans (both men and women). This type of growth develops in the colon or the rectum, also known as large intestine. According to recent reports from “the American Cancer Society”, more than 136,830 people will be diagnosed with CRC and about 51, 310 people will die from this disease in the year 2014.
The lifetime risk of developing this condition is about 1 in 20 (5%) and this is somewhat lower in women than in men. However, this may vary broadly according to individual risk factors. It is estimated that about 72% cases develop in the colon and 28% in the rectum. The potential risk factors associated with this disease include age, family history or genetic factors, lifestyle related factors such as diet, smoking, physical inactivity, obesity or alcohol use.
Screening for Colorectal Cancer – Importance
Generally, people in the early stages of this disease do not have any specific symptoms, but as the disease advances the symptoms become more evident. The nature of signs and symptoms may vary from one person to another. Some of the main symptoms include unexpected weight loss, abnormal bowel habits, cramping or stomach discomfort, vomiting, diarrhea, constipation, and a feeling of weakness or fatigue. In addition, the intensity of symptoms may be different from one person to another and will vary in severity.
With regular screening, CRC can be diagnosed early, when it is most likely to be curable. In most cases, routine screening helps in finding the growth of small polyps and removing them before they becom cancerous. Early detection of symptoms may lead to more effective treatment resulting in high survival rates.
It is essential for people (who have no identified risk factors other than age) to begin regular screening at an early age. On the other hand, those who have a family history or other potential risk factors for colorectal polyps must discuss with their physicians about the need for frequent screening. Different tests are used to detect the disease symptoms in its early stages and these include – colonoscopy, sigmoidoscopy, guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT), CT colonography (virtual colonoscopy) and stool DNA test.
As per the recommendations of the “American Cancer Society”, both men and women (at the age of 50) who are at average risk for developing CRC should perform one of the screening tests given below –
- Flexible sigmoidoscopy every 5 years
- Double-contrast barium enema every 5 years
- CT colonography (virtual colonoscopy) every 5 years
- Colonoscopy every 10 years
High Rates of Colorectal Cancer in Young Adults – Finds a Study
The general incidence and mortality rates of colorectal cancer (CRC) have been decreasing in the United States, a trend that is mainly related to the extensive screening of patients aged 50 years and older. However, a new study (conducted by researchers from the University of Texas MD Anderson Cancer Center in Houston) found that the incidence of this disease is increasing among young adults (particularly those in the age group of 20-34 years). The study results published in the online issue of JAMA Surgery (November 5, 2014) found a higher increase in the incidence of colon and rectal cancer at all stages (localized, regional and distant).
As part of the study, researchers analyzed the data of the National Cancer Institute (NCI) between the years 1975-2010 and found that the incidence of this condition has reduced by one percent per year for both men and women. It was also found that the overall age-adjusted incidence rates decreased by 0.92%.
Even though there existed significant differences in the rate of diagnosis when it comes to age, researchers found that the occurrence of colon cancer has reduced by 1 % per year in older people above 50 years of age and increased by 2% per year in people between 20-34 years of age. It is estimated that if this trend continues, by the end of 2030 the prevalence of this condition will significantly increase by 90% among younger adults (between 20-34 years of age). Some of the other major findings of the study include –
- The incidence rate for rectosigmoid and rectal cancers increased by 49.7% and 124.2% respectively among younger adults.
- For those people aged between 35-49 years, the incidence rates increased at a slow pace – 27.7% for colon and 46% for rectal cancer by the end of 2030.
The study results indicate a steady increase in incidence rate in younger adults over the past few years. In fact, the reports suggest that 1 out of 6 cases of colon cancer and 1 out of 4 cases of rectal cancer occur in patients below 50 years.
Researchers say that it is quite impossible to analyze and determine the exact causes related to the increase in incidence rates among younger adults (especially people between 20-34 years of age). Some of the potential factors could be related to lifestyle, dietary and other environmental factors. On the other hand, behavioral factors such as obesity and physical inactivity may also play a pivotal role for this significant increase.
Reports suggest that the current screening programs do not target the younger population. However, if these increasing trends are likely to continue, a doubling of colon cancer rates can be witnessed within the next 15 years. Delay in early detection of disease symptoms can be regarded as one possible cause for this increasing trend. In most cases, young adults may not undergo routine screening programs until there is a valid reason for it like history of familial polyps. Moreover, before the introduction of the Affordable Care Act, many patients lacked health insurance coverage, which may have delayed diagnosis.
The study signifies the need to devise effective strategies for early detection and prevention of this health condition. All colorectal cancers may not be the same and the nature of this disease may be different and it could be that young patients may have another subtype. Hence, an ideal solution for patients is to seek adequate care and for healthcare providers to consider CRC as part of a differential diagnosis in order to avoid the possible delay. It is important for people to follow a healthy lifestyle by giving equal importance to both exercise and diet.