Accurate medical billing plays an integral role in the financial success of any healthcare practice, and gastroenterology is no exception. Due to the complex nature of gastrointestinal procedures such as endoscopy, colonoscopy, and biopsy and coding requirements, gastroenterologists often face distinct billing challenges. Even minor billing errors can lead to claim denials, compliance issues, or revenue loss. Following the right gastroenterology billing guidelines is therefore crucial for every practice looking to optimize revenue cycle, minimize errors, and remain compliant with evolving healthcare regulations. This article explores the top billing guidelines and best steps that gastroenterology practices can follow to streamline the entire process.
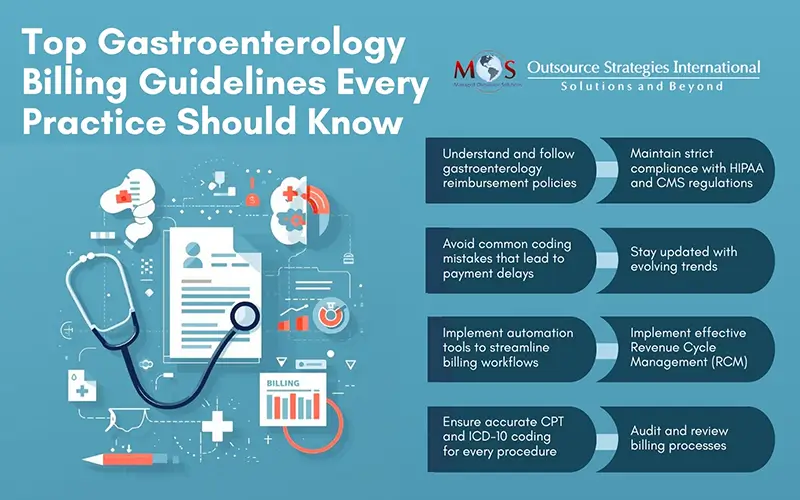
Steps to Streamline Gastroenterology Billing Processes
According to a recent report by Precedence Research, the global gastroenterology market was valued at USD 54.56 billion in 2023 and is projected to reach USD 93.8 billion by 2032. This significant growth is primarily driven by the rising incidence of gastrointestinal disorders linked to unhealthy dietary habits, advancements in clinical research, escalating healthcare expenditures, and an expanding elderly population.
- Understanding Gastroenterology Billing Guidelines
Following gastroenterology billing guidelines ensures that every service rendered is accurately coded and billed according to payer requirements. Healthcare practices should pay close attention to documentation. Each procedure note must clearly outline the medical necessity, scope, and findings of the service provided. For instance, when billing for an upper endoscopy, detailed reports of the esophagus, stomach, and duodenum should be included to support the claim. Missing or incomplete documentation often results in claim rejection or reduced reimbursement. Additionally, understanding payer-specific rules is critical. Different insurance carriers have varying coverage policies for procedures such as colon cancer screenings, polyp removals, and capsule endoscopies. Staying updated with these rules helps reduce the risk of denials and ensures compliance with payer-specific gastroenterology reimbursement policies.
- Ensure Accurate Use of CPT and ICD-10 Codes
Accurate coding is the foundation of successful billing. Misuse or omission of codes can result in underpayments or compliance audits. Some of the most common procedures in gastroenterology include –
- Colonoscopy (45378–45398)
- Upper GI Endoscopy (43235–43259)
- ERCP (43260–43278)
- Capsule Endoscopy (91110–91111)
Each code represents a different complexity level and must be supported by appropriate documentation. For example, when a gastroenterologist removes a polyp during a colonoscopy, the CPT code changes to reflect both diagnostic and therapeutic intent. Professional gastroenterology medical billing and coding services can help practices ensure coding precision, prevent up coding or under coding.
- Avoid Common Coding Mistakes in Gastroenterology Billing
Even experienced billing staff can make errors that impact the practice’s bottom line. Being aware of common coding mistakes in gastroenterology billing can prevent unnecessary revenue loss. Some of the most common billing errors in gastroenterology include –
- Incorrect modifier usage – Modifiers such as 25, 26, and 59 must be applied correctly to indicate separate and distinct services.
- Improper linkage between diagnosis and procedure codes – Each procedure must be supported by a relevant ICD-10 code that justifies medical necessity.
- Billing for incomplete procedures – If a procedure is cancelled or partially completed, the documentation and coding must reflect this accurately.
- Duplicate billing – Submitting claims for the same service multiple times can trigger audits and payer penalties.
Implementing regular internal audits and working with expert billing professionals will help identify these issues early and maintain claim accuracy.
Reduce denials and maximize profitability!
For specialized medical billing services
- Follow Gastroenterology Reimbursement Policies
Understanding gastroenterology reimbursement policies is vital for maximizing payment outcomes. Each payer, whether Medicare, Medicaid, or private insurers, has unique reimbursement methodologies. For instance, preventive colonoscopies may be reimbursed differently than diagnostic ones, depending on whether polyps are found and removed. Medicare has specific screening guidelines that must be adhered to. Failing to differentiate between screening and diagnostic codes may result in incorrect payment.
Practices should also stay informed about bundled payment structures and value-based care initiatives. Some insurers may group related procedures under a single payment, requiring detailed documentation to ensure appropriate reimbursement. Professional gastroenterology medical billing and coding services can help practices stay compliant with changing reimbursement policies and avoid costly delays.
- Implement Effective Revenue Cycle Management (RCM)
A strong revenue cycle management process ensures that all claims are processed, paid, and reconciled efficiently. Gastroenterology practices should focus on end-to-end RCM strategies – from patient registration to final payment posting. Key steps include –
- Eligibility verification – Confirm patient insurance coverage before performing procedures.
- Accurate charge entry – Ensure all services are recorded promptly and coded accurately.
- Claim submission and tracking – Submit claims electronically and follow up on pending or denied claims regularly.
- Payment posting and reconciliation – Record payments accurately to identify underpayments or unpaid claims.
By leveraging automation tools and gastroenterology medical billing and coding services, practices can significantly improve claim turnaround times and reduce administrative burden.
- Maintain Compliance with Healthcare Regulations
Gastroenterology billing is governed by strict compliance standards from organizations like HIPAA, CMS, and the Office of Inspector General (OIG). Violations can lead to audits, fines, and reputational damage. Practices must ensure compliance by –
- Conducting regular staff training on new billing and coding updates
- Maintaining secure patient records and protecting PHI (Protected Health Information)
- Performing internal audits to detect and correct compliance issues
- Following payer-specific documentation guidelines
Following regulatory updates and payer rules can help maintain compliance and reduce legal risks.
- Remain Updated with Evolving Billing Trends
The healthcare billing landscape is continually evolving, and gastroenterology practices must adapt to changes such as AI-driven billing tools, telehealth reimbursement models, and real-time claim tracking systems. By integrating advanced technologies, practices can automate repetitive tasks, enhance accuracy, and improve efficiency. Reliable gastroenterology medical billing and coding services often employ these tools to ensure claims are submitted correctly and payments are received faster.
- Regularly Audit and Review Billing Processes
Routine audits are essential for identifying discrepancies, minimizing revenue leakage, and ensuring compliance with gastroenterology billing guidelines. Internal audits should focus on reviewing documentation accuracy, modifier use, denied claim trends, and payer-specific coding requirements. Auditing not only prevents financial loss but also helps identify staff training needs. By addressing recurring mistakes and updating coding practices, gastroenterology practices can maintain a high level of accuracy in billing operations.
Following proper billing guidelines is not just about compliance – rather it is about building a sustainable financial framework for your practice. With detailed documentation, accurate coding and a thorough understanding of gastroenterology reimbursement policies, practices can avoid common billing errors and ensure faster claim approvals.
Given the increasing complexity of medical billing, many gastroenterology providers are turning to professional gastroenterology medical billing and coding services for expert assistance. These specialized services help streamline workflows, reduce administrative errors, and improve overall revenue performance. By focusing on accuracy, compliance, and continuous process improvement, your gastroenterology practice can deliver high-quality patient care without the burden of billing complications.
Empower Your Practice with Smart Billing Solutions!
Enhance accuracy, compliance, and profitability with our expert billing services.