Orthopedic practices perform a wide range of joint surgeries, musculoskeletal treatments, ligament reconstructions, and spinal interventions. Managing prior authorization in orthopedic billing is challenging, as requirements vary across surgeries, procedures, therapies, medications, and injections. Obtaining timely approvals from insurance companies is crucial because orthopedic procedures are often complex and costly. Moreover, delays in orthopedics insurance verification may directly affect patient mobility, pain management, and long-term health outcomes in some cases, leading to setbacks in recovery. Managing this task with an in-house team is time-consuming and prone to errors, so many practices turn to insurance authorization and verification services to streamline the process.
What Is Prior Authorization in Orthopedic Billing?
Prior authorization is a formal approval process required by the insurance companies before certain medical services can be performed or billed. In orthopedics, this typically applies to procedures that involve surgical interventions, specialized therapies, advanced imaging, or high-cost medications. The goal of this prerequisite is to confirm that the proposed orthopedic treatment is medically necessary, aligns with payer guidelines, and qualifies for reimbursement coverage.
Beyond its definition, orthopedic insurance approvals operate as the financial gatekeeper of the revenue cycle. Every request must be supported with precise clinical notes, diagnostic details, and coding that matches payer requirements. Even minor discrepancies can trigger delays, rejections, or additional information requests. As a result, health plan approval not only shapes care access but also directly influences operational efficiency, cash flow, and financial stability of a practice.
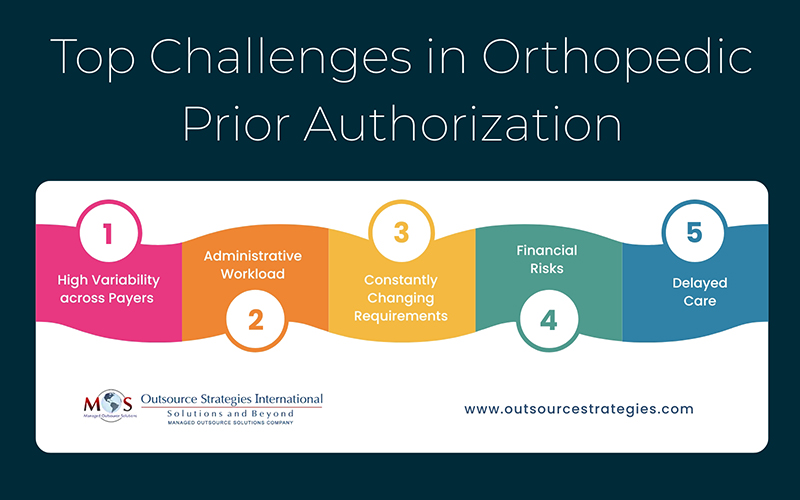
Main Challenges of Orthopedic Insurance Approvals
Orthopedic practices already balance high patient volumes and complex treatment plans, but the insurance approval process adds another layer of difficulty. Payers have their own rules, timelines, and forms, often requiring as many as 20 staff hours per week just to secure approvals before a patient even enters the facility.
The challenge is further compounded by constant changes in payer requirements. Coverage criteria can shift with little notice, and insurers frequently request additional details or clarifications. This forces providers to divert time and attention away from direct patient care and creates an environment where delays and insurance claim denials are difficult to avoid. Together, these factors increase administrative workload, drive up operational costs, and heighten the risk of compliance issues. Effective orthopedic revenue cycle management is critical to mitigating these challenges.
Let’s go through the main challenges orthopedic practitioners face in getting approvals:
- High Variability across Payers
Each insurance company, be it Medicare, Medicaid, or commercial, sets its own requirements for prior authorization, and no two sets of rules are ever quite the same. What one payer accepts for ligament reconstruction billing may not be sufficient for another. This lack of standardization means billing teams must constantly juggle different sets of rules and spend extra time double-checking guidelines, even for similar procedures. This inconsistency increases the risk of missed details and denials.
- Administrative Workload
The process of collecting records, filling out forms, and submitting requests for approvals can consume hours of staff time. Each pre-authorization process request must be handled carefully to avoid delays. Orthopedic documentation, coding, and billing guidelines involve multiple body parts, techniques, and implants, demanding hours of paperwork to submit even a single authorization request.
In case of a rejection or denial, the billing team must often spend additional time correcting errors or appealing the decision. This administrative burden can pull resources away from more strategic tasks that directly support patient care.
- Constantly Changing Requirements
Insurance rules and authorization policies constantly evolve as payers update coverage criteria to control costs and align with updated clinical guidelines. What is acceptable one month may be outdated the next, forcing billing teams to constantly monitor updates from multiple payers. This ongoing need for vigilance adds even more strain to already limited resources, especially for smaller clinics. Even a small oversight, such as missing a newly added diagnosis code, can cause an entire request to be denied.
- Financial Risks
Missed or denied payer approvals often come with significant financial consequences. Practices may be forced to resubmit claims, provide additional documentation, write off procedures, or in some cases, take on the full expenses of the service. These disruptions not only negatively affect the revenue cycle but can also reduce the resources available for investing in staff, technology, equipment, and patient care improvements.
- Delayed Care
Even when authorization forms are submitted correctly, approval timelines can vary greatly between insurers. Patients waiting for critical procedures like spinal surgeries, joint replacements, or ligament repairs may face weeks of uncertainty before care can begin. These delays directly affect mobility, pain management, and overall recovery, while also straining the trust patients place in their provider.
Best Practices for Pre-authorization in Orthopedic Clinics
Getting prior authorizations approved on time is not easy, but with consistent process improvements, healthcare providers can increase efficiency, lower denials, and keep patients on schedule for the care they need. Here are the best practices that providers can implement to optimize operations and deliver timely care.
- Dedicated Team
Establish a management team by assigning tasks to specific team members for effectively handling prior authorization. Specialized team members can focus solely on insurance authorization tasks such as verifying coverage details, completing payer-specific forms, and following up on outstanding requests. Practices can develop a robust insurance authorization strategy to systematically approach each case, ensuring consistent, accurate, and timely submissions. With a dedicated team, you can reduce clinical errors, prevent delays in care, and free up other staff to focus better on strategic initiatives.
- Leverage Technology and Automation
Manually tracking every authorization request across different payers is not only slow, but also prone to errors. Orthopedic practices can address this issue by adopting advanced pre-authorization tools. These tools can be integrated with electronic health records (EHRs) and billing systems to automate parts of the authorization process. Automating routine workflows such as eligibility verification, form filing, and status tracking can reduce human errors and shorten turnaround times, improving overall efficiency of the pre-encounter billing workflow.
- Standardize Documentation and Coding
Creating a standardized template for documentation and coding can help ensure that every prior authorization request contains all required information. This includes medical history, imaging results, procedure codes, and relevant notes from the orthopedic surgeon. Consistency in documentation reduces the likelihood of denials due to missing or incomplete information and enhances the accuracy of the approval process.
- Proactive Communication with Payers
Building a proactive relationship with insurance representatives can pay dividends in the long term. Regular communication with payers helps to understand their specific requirements, address potential issues before they escalate, and expedite approvals. By maintaining a clear communication channel between orthopedic specialists, pre-authorization team, and payers, practices can minimize confusions and potential delays for patients with critical orthopedic needs.
- Monitor and Analyze Denials
Tracking patterns in authorization denials provides valuable insights into process bottlenecks and potential areas of improvement. Recording and analyzing denial data helps to find root causes such as missing documentation, incorrect coding, or outdated payer criteria. Based on these findings, practices can develop and implement corrective measures, refine workflows, and prevent repeated errors. A data-driven approach not only improves efficiency but also protects the practice’s revenue cycle.
By applying these practices consistently, orthopedic clinics can simplify the insurance authorization process, reduce administrative complexities, ensure faster approvals, and ensure better patient outcomes. Given the challenges of internally managing the approval process, utilizing insurance authorization services has emerged as a practical solution for orthopedic practices.
Get faster claim approvals with our expert orthopedic billing services!