Mental health care professionals work in tandem with primary care providers to ensure that the clinical goals of the patient are met. Collaborative care model has proved to be effective in cutting costs, with improved access and clinical outcomes. In 2017, the Centers for Medicare and Medicaid Services (CMS) approved the payment for services that are provided to patients with behavioral health disorders (including substance use disorder). There are patients who participate in psychiatric collaborative care programs or who receive behavioral health integration services. These groups of services are classified by CMS as “Behavioral Health Integration”) (BHI) services.
Psychiatric Collaborative Care Management Services (CoCM) are billed using the three codes: 99492, 99493 and 99494. General BHI service is coded as 99484. The treating physician or Primary Care Provider is required to submit the claims for these services. A physician coding company ensures timely submission of claims so that physicians can offer seamless experience to their patients without the hassle of classifying between Chronic Care Management services and Behavioral Health Integration Services. Accurate coding and timely submission of claims are essential for health practitioners to effectively track the health records of the patients and receive medical reimbursement.
Psychiatric Collaborative Care Services model
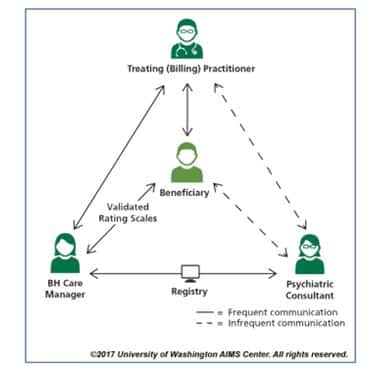
Primary health care is enhanced by Behavioral Health Integration services, particularly for patients whose conditions are not improving.
The treatment strategy of this model involves:
- Offering care management support for patients receiving behavioral health treatment
- Frequent consultation by inter-specialty psychiatrist
- Delivering CoCM by Behavioral Health Care Manager, the Psychiatric Consultant and Treating ( Billing) Practitioner
CPT codes used to bill for CoCM
99492: Initial psychiatric collaborative care management, first 70 minutes in the first calendar month of behavioral health care manager activities, in consultation with a psychiatric consultant, and directed by the treating physician or other qualified health care professional, with the following required elements:
- Outreach to and engagement in treatment of a patient directed by the treating physician or other qualified health care professional
- Initial assessment of the patient, including administration of validating rating scales, with the development of an individualized treatment plan
- Review by the psychiatric consultant with modifications of the plan if recommended
- Entering patient in a registry and tracking patient follow-up and progress using the registry, with appropriate documentation, and participation in weekly caseload consultation with the psychiatric consultant
- Provision of brief interventions using evidence-based techniques such as behavioral activation, motivational interviewing and other focused treatment strategies.
99493: Subsequent psychiatric collaborative care management, first 60 minutes in a subsequent month of behavioral health care manager activities, in consultation with a psychiatric consultant, and directed by the treating physician or other qualified health care professional, with the following required elements:
- Tracking patient follow-up and progress using the registry, with appropriate documentation
- Participation in weekly caseload consultation with the psychiatric consultant
- Ongoing collaboration with and coordination of the patient’s mental care with the treating physician or other qualified health care professional and any other treating mental health providers
- Additional review of progress and recommendations for changes in treatment, as indicated, including medications, based on recommendations provided by the psychiatric consultant
- Provision of brief interventions using evidence-based techniques such as behavioral activation, motivational interviewing, and other focused treatment strategies
- Monitoring of patient outcomes using validated rating scales; and relapse prevention planning with patients as they achieve remission of symptoms and/or other treatment goals and are prepared for discharge from active treatment.
99494: Initial or subsequent psychiatric collaborative care management, each additional 30 minutes in a calendar month of behavioral health care manager activities, in consultation with a psychiatric consultant, and directed by the treating physician or other qualified health care professional. The billing of these codes is based on the amount of time the behavioral health care manager spends doing clinical work (face-to-face and non face-to-face) with the patient.
99484: It is used to bill monthly services other than CoCM.
Clinical staff members spend at least 20 minutes each month coordinating and managing a patient’s behavioral health services under the direction of a physician or other qualified health care professional.
Health care practitioners can seek medical coding services to correctly code for the services provided. Trained coders are up-to date with the latest billing codes. By outsourcing medical coding requirements, errors in billing can be considerably reduced thereby eliminating claim rejections. Also, revenue cycle can be effectively managed while giving utmost priority to patient care.




