- Medical Coding for In Vitro Fertilization (IVF) Treatments
- ICD-10 Codes
- ICD-10 Codes for ART procedures
- CPT Codes
- HCPCS Codes
- What to Know about In-Vitro Fertilization Verifications and Authorizations?
- IVF Insurance Verification
- Prior Authorization for Infertility Treatment
- Steps to Obtain Preauthorization for IVF Treatment
In vitro fertilization (IVF), the most common type of assisted reproductive technology (ART), enables many couples for whom other infertility treatments have not worked, achieve a pregnancy. Medical billing and coding services for In vitro fertilization (IVF) treatment involve documenting this procedure on your medical claims using a complex and specialized set of diagnosis and procedure codes. Gynecologists and fertility specialists can accurately report their services and the diagnoses that justifies them with the support of reproductive medicine billing and coding services. Treatments for infertility range from simple interventions such as fertility drugs to induce ovulation to more complicated options such as artificial insemination or IUI sperm injections and in vitro fertilization (IVF).
Medical Coding for In Vitro Fertilization (IVF) Treatments
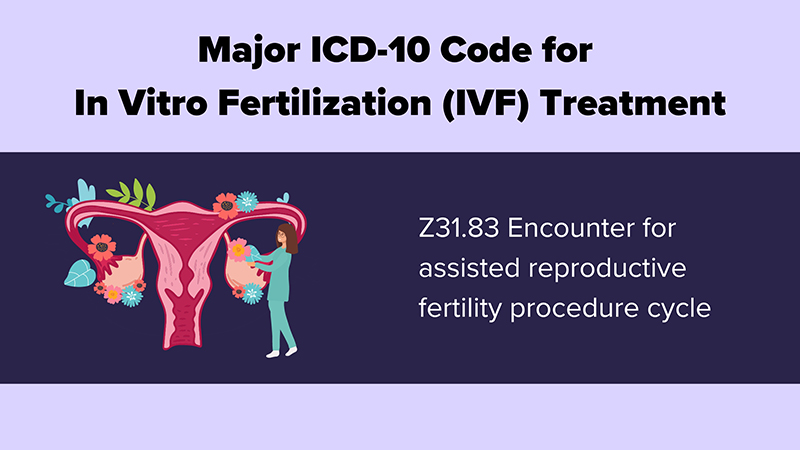
ICD-10 Codes
Types of IVF are coded under Z31.83
- Z31 Encounter for procreative management
- Z31.0 Encounter for reversal of previous sterilization
- Z31.4 Encounter for procreative investigation and testing
- Z31.41 Encounter for fertility testing
- Z31.42 Aftercare following sterilization reversal
- Z31.43 Encounter for genetic testing of female for procreative management
- Z31.44 Encounter for genetic testing of male for procreative management
- Z31.49 Encounter for other procreative investigation and testing
- Z31.5 Encounter for procreative genetic counseling
- Z31.6 Encounter for general counseling and advice on procreation
- Z31.61 Procreative counseling and advice using natural family planning
- Z31.62 Encounter for fertility preservation counseling
- Z31.69 Encounter for other general counseling and advice on procreation
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z31.8 Encounter for other procreative management
- Z31.81 Encounter for male factor infertility in female patient
- Z31.82 Encounter for Rh incompatibility status
- Z31.83 Encounter for assisted reproductive fertility procedure cycle
- Z31.84 Encounter for fertility preservation procedure
- Z31.89 Encounter for other procreative management
- Z31.9 Encounter for procreative management, unspecified
ICD-10 Codes for ART procedures
- O09.81 Supervision of pregnancy resulting from assisted reproductive technology
- O09.811 …… first trimester
- O09.812 …… second trimester
- O09.813 …… third trimester
- O09.819 …… unspecified trimester
CPT Codes
- 58970 Follicle Puncture for Oocyte retrieval, any Method (IVF)
- 89250 Culture of oocyte(s)/embryo(s), less than 4 days
- 89251 Culture of oocyte(s)/Embryo(s), less than 4 days; with co-culture of oocyte(s)/embryo(s)
- 89253 Assisted embryo hatching, microtechniques (any method)
- 89254 Oocyte identification from follicular fluid
- 89255 Preparation of embryo for transfer (any method)
- 89257 Sperm identification from aspiration (other than seminal fluid)
- 89260 Sperm isolation; simple prep (e.g. spermwash and swim-up) for insemination or diagnosis with semen analysis
- 89261 Sperm isolation; complex prep (e.g Percoll gradient, albumin gradient for insemination or diagnosis with semen analysis
- 89268 Insemination of oocytes
- 89272 Extended culture of oocyte(s)/embryo(s), 4-7 days
HCPCS Codes
- S4011 In vitro fertilization; including but not limited to identification and incubation of mature oocytes, fertilization with sperm, incubation of embryo(s), and subsequent visualization for determination
- S4015 Complete in vitro fertilization cycle, not otherwise specified, case rate
- S4016 Frozen in vitro fertilization cycle, case rate
- S4017 Incomplete cycle, treatment canceled prior to stimulation, case rate
- S4018 Frozen embryo transfer procedure canceled before transfer, case rate
- S4020 In vitro fertilization procedure canceled before aspiration, case rate
- S4021 In vitro fertilization procedure canceled after aspiration, case rate
- S4022 Assisted oocyte fertilization, case rate
- S4023 Donor egg cycle, incomplete, case rate
- S4025 Donor services for in vitro fertilization (sperm or embryo), case rate
- S4026 Procurement of donor sperm from sperm bank
- S4028 Microsurgical epididymal sperm aspiration (MESA)
- S4037 Cryopreserved embryo transfer, case rate
It is important to note that medical codes are updated regularly, and healthcare providers as well as their billing staff must stay up-to-date with the latest changes. This ensures that the correct codes are used, and that insurance claims are not denied due to outdated codes. Accurate record-keeping and billing are also essential for both individual patient care and the advancement of healthcare as a whole.
What to Know about In-Vitro Fertilization Verifications and Authorizations?
Coverage for infertility treatment varies widely among insurance plans and among states. Insurance verifications and authorizations are an essential part of providing reproductive medicine treatment for insured patients seeking fertility treatment. Insurance companies use very specific guidelines to determine the extent of each member’s infertility benefits and how their claims will be processed. For example, Cigna’s policy for infertility injectables states: “When coverage is available and medically necessary, the dosage, frequency, duration of therapy, and site of care should be reasonable, clinically appropriate, and supported by evidence-based literature and adjusted based upon severity, alternative available treatments, and previous response to therapy”.
IVF Insurance Verification
Insurance verification involves verifying a patient’s eligibility for these services. Eligibility issues are the one of the most common reasons for claim denials. IVF verifications are critical before starting the treatment cycle to enable the patient to understand what the insurance plan will cover and for the provider to submit accurate claims. Partnering with an insurance verification company is the best option for infertility specialists to carry out this important but tedious task.
In-vitro verifications will validate the following:
- Patient demographic information
- Type of plan
- Claims mailing address
- Whether the provider is in the insurance plan’s network
- Patient’s financial responsibility: copays, deductibles and out-of-pocket limits
- Patient policy status
- Effective date
- Payable benefits
- Plan exclusions
- Insurance caps
- Primary and secondary insurers
- Out of network benefits
- Referrals and pre-authorizations
In addition to this basic information, the following are also verified:
- Infertility benefits as well as any benefit exclusions
- Whether specific medical criteria should be met to be eligible for infertility benefits
- Whether the plan requires a documented diagnosis
- Whether the patient should undergo lesser treatments (IUI) before proceeding to advanced treatments (IVF/ICSI)
- Whether IVF/ICSI only be paid for certain diagnoses
- If there is any limit, dollar or number, on treatment cycles
- If there are any factors that would cause denial of benefits, for e.g. prior failed treatment, prior sterilization
- Coverage for male infertility diagnosis and infertility care
- Lifetime maximums for infertility treatment
Prior Authorization for Infertility Treatment
Most health insurance companies require providers to obtain approval from the patient’s plan before they will cover the costs of a specific medicine, medical device or procedure. Completing prior authorization or pre-authorization requirements is a key process to avoid claim denials.
Many insurance plans require prior authorization, precertification, or registration with infertility case management when it is determined that infertility treatment is appropriate. After the provider and patient agree on a treatment plan, in-network infertility specialists have to determine what infertility treatments, medications, and procedures are covered under the patient’s health plan.
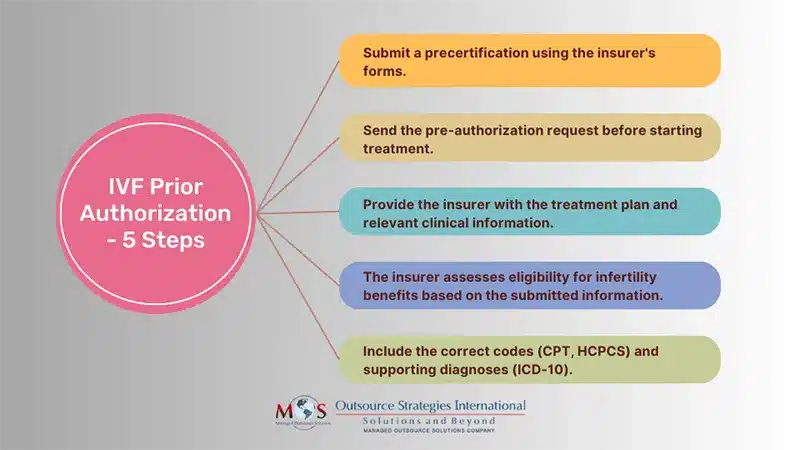
Steps to Obtain Preauthorization for IVF Treatment
- The provider has to submit a precertification using the insurer’s designated request forms.
- The pre-authorization request should be submitted before the treatment is started.
- The treatment plan should be submitted to the insurer along with any pertinent clinical information.
- The health insurer will use the information submitted by the provider to determine if the patient is eligible to access the applicable infertility benefit.
- The requested services or procedures should be submitted with the appropriate CPT and ICD-10 Code
Estimates for patient responsibility such as deductibles and co-insurance are not typically included in the cost calculation. For example, United Healthcare usually pays around 80% in cost-sharing plans and the patient may have to pay for 20% of covered fertility services. Preauthorization for IVF procedures generally takes about 1-2 weeks. Medication preauthorization may be obtained faster.
Medical billing companies with expertise in infertility and reproductive endocrinology medical billing and coding can help gynecology practices overcome coding and claim submission challenges. This will allow providers to focus on helping patients overcome their fertility challenges.