Medical billing involves translating healthcare services into billing codes and submitting claims to insurance companies for reimbursement. Errors can be costly. Did you know that medical billing errors cost the U.S. healthcare system billions of dollars each year?
Accurate and timely billing and claim submission is crucial to optimize revenue. That’s where a medical billing company comes in. An efficient company helps healthcare providers manage and optimize their billing process, ensuring accurate claims submission, quicker reimbursements, and improved revenue cycle management (RCM).
Considering outsourcing your medical billing? Medical billing and coding services for physicians will help ensure that every diagnosis and treatment is accurately represented, leading to fewer errors and faster reimbursement.
Let’s delve into the functions of medical billing outsourcing companies, the comprehensive services they offer, and how choosing a reliable partner can enhance your revenue, streamline processes, and cut administrative costs.
Comprehensive Suite of Services Provided by Medical Billing Companies
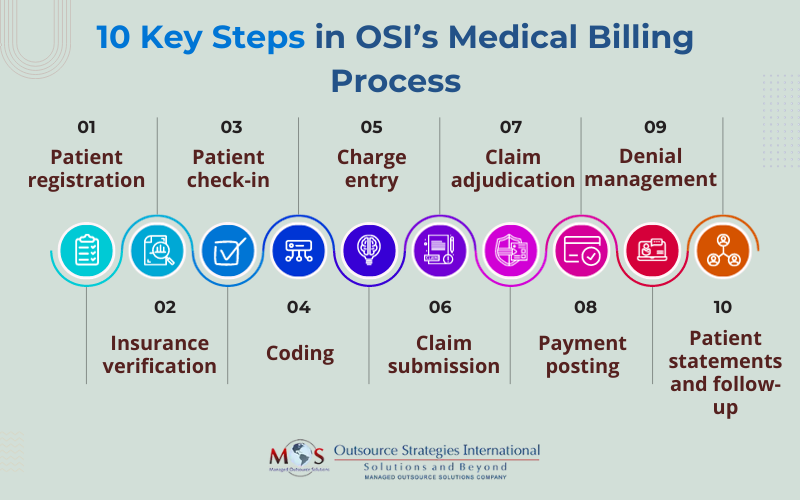
Experienced outsourcing companies manage the entire billing, coding and claim submission process efficiently, helping healthcare providers submit error-free, timely claims.
The services offered by an experienced medical billing company cover:
- Enrollment into the billing system: This first step in the billing process and crucial for accurate billing and claims submission. It involves gathering and verifying patient-specific details, including demographics, insurance details, and consent during the registration process. Electronic enrollment streamlines the process and enables insurance companies to obtain necessary data about the patients with just a click of the mouse on a single screen.
- Eligibility verification and prior authorization: Patient eligibility verification ensures that patients have valid insurance coverage by confirming details such as policy status and coverage limits. Prior authorization is a necessary step where healthcare providers obtain approval from insurance companies before performing certain medical procedures or treatments, helping ensure coverage and prevent potential claim denials.
- Insurance verification: Professional companies manage the verification procedures efficiently. They confirm patients’ active medical coverage with the insurance company, including type of plan, policy status, effective date, plan exclusions, claims mailing address, patient responsibilities comprising co-pays, co-insurances and deductibles, and much more.
- Prior authorization: Certain medical services and procedures require approval from the insurer before they are provided. Obtaining insurance authorization is a time-consuming task. A medical billing company will submit prior authorization requests and help implement best practices to manage the process.
- Medical coding: Medical billing companies also ensure precise medical coding to communicate details of the healthcare services rendered. Their experienced certified coders carefully analyze patient records, clinical notes, and other relevant documentation to assign accurate Current Procedural Terminology (CPT), International Classification of Diseases (ICD-10), and Healthcare Common Procedure Coding System (HCPCS) codes. Systematic coding ensures that billed services are accurately represented, facilitating smoother claim submissions to insurance companies and reducing the chances of errors or rejections in the billing process.
- Billing and reconciling of accounts: This involves verifying that payments made by insurance companies match the billed amounts, ensuring accuracy in the financial transactions. The aim is to reconcile any discrepancies or differences in the accounts and ensure accurate and up-to-date financial records for both the healthcare provider and the patient. The process includes
- Charge entry
- Payment posting
- Reconciliation
- Accounts receivable collections: This systematic process involves managing and collecting outstanding payments from patients, insurance companies, or other third-party payers for healthcare services rendered. Outsourcing companies handle the AR collection process efficiently, following up on unpaid claims, sending reminders or inquiries to insurers and patients, negotiating settlements, and ensuring that outstanding balances are collected in a timely manner.
- Audits: The primary goal of a medical billing audit is to identify any discrepancies, errors, or potential fraudulent activities. This comprehensive assessment usually involves a thorough examination of patient records, coding practices, billing documentation, and adherence to healthcare coding standards. Specialists audit the charges entered by the charge team to assess accuracy in data entry and adherence to billing regulations. They also verify claim accuracy according to carrier specifications, ensuring compliance with billing rules.


Ready to Boost Revenue?
Talk to us today at (800) 670-2809 and discover the benefits of outsourcing your medical billing!
Choose a Professional Medical Billing Company
If you are looking to outsource your RCM process, choose a partner that prioritizes accuracy and ensures customized solutions in minimum turnaround time.
Factors to Consider When Choosing a Medical Billing Company
- Expertise and experience
- HIPAA compliance and security measures
- Expert team
- Technology
- Customization and flexibility
- Quality assurance practices
- Fast turnaround time
- Cost transparency
- Communication and reporting
- Client testimonials and reviews

With a wealth of experience and a proven track record, OSI consistently delivers tangible results for our diverse healthcare specialty clients. Our team can provide comprehensive RCM solutions or tailored strategies to meet client needs.





