Endometrial hyperplasia is a condition where the lining of the uterus thickens, leading to heavy or abnormal bleeding. Billing and coding for gynecology conditions can be complex, but professional medical billing outsourcing companies can assist in managing claim submissions for timely reimbursement. There are two types of endometrial hyperplasia: without atypia, which doesn’t involve unusual cells, and atypical endometrial hyperplasia, which is considered precancerous due to the presence of abnormal cells. Diagnosis may involve evaluating medical history and performing tests such as transvaginal ultrasound, hysteroscopy, and biopsy. Treatment options include hormone therapy (progestin) or surgery. In severe cases or when cancerous cells develop, a hysterectomy (uterus removal) may be recommended.
Accurate medical documentation is crucial for reporting endometrial hyperplasia, ensuring clear support for diagnosis and detailed procedure descriptions. It should establish medical necessity, including symptom descriptions, failed conservative treatments, or the severity of the condition.
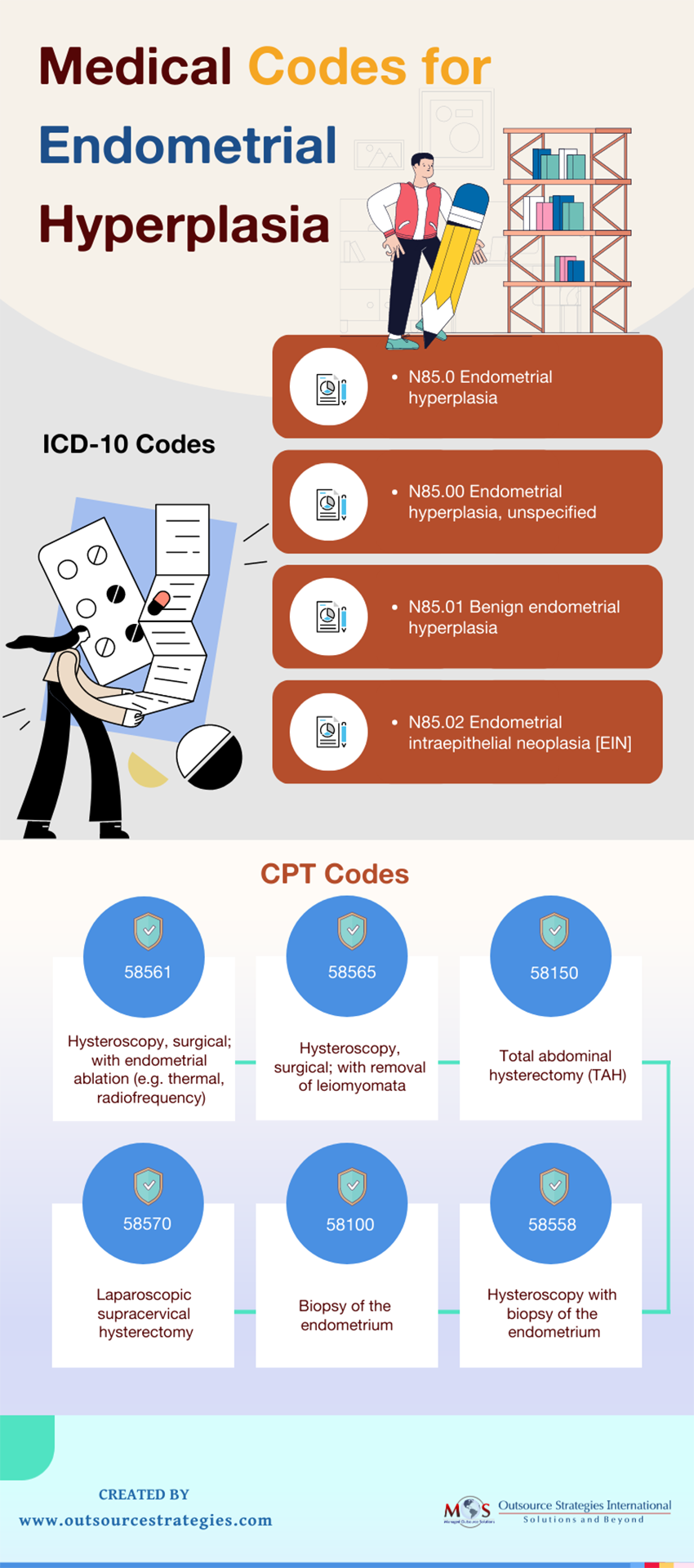
Healthcare providers should stay updated on relevant medical codes for reporting endometrial hyperplasia accurately. Outsourcing medical billing tasks to providers of billing services ensures correct and timely claim submissions for optimal reimbursement.
Eliminate billing headaches and embrace streamlined processes.
Discover the benefits of outsourcing today!
Check out the infographic below