Ever-changing regulations, complex reimbursement trends and shifting payer landscapes have made effective dental revenue cycle management (RCM) foundational for a practice’s financial success. Dental RCM is a comprehensive process that covers all administrative and clinical functions, starting from patient scheduling and insurance verification, to claims submission and the collection of final payment. When the process is optimized, the dental billing process is completed efficiently, ensuring timely reimbursement, reduced administrative burdens, and minimal cash flow disruptions. On the other hand, inefficiencies in the dental RCM workflow can result in substantial financial losses, which is why many dental practices rely on professional support to protect profitability and ensure long-term sustainability. Learn how dental RCM works, how to build an efficient dental RCM workflow, and why it’s important to your practice.
Dental RCM vs. Dental Billing: Understanding the Difference
While these terms are often used interchangeably, there are some basic differences between them. Dental billing is only a part of the RCM and covers the specific processes of claim creation and submission, collecting co-pays and deductibles from patients, and posting payments. RCM is a broader strategy, covering the entire financial journey of a patient, from the moment an appointment is scheduled until the final payment is collected.
Outsource your dental RCM and focus on patient care while we handle your revenue cycle from start to finish!
Key Components of an Effective Dental RCM Workflow
In a dental practice, an effective RCM workflow comprises several front-end and back-end processes that work together to ensure smooth financial operations. Front-end processes occur before patient services, focusing on patient engagement and information gathering. The Medical Group Management Association (MGMA) reports that front-office efficiency plays a critical role in shaping billing and collection outcomes, directly affecting the overall success of a healthcare facility. Back-end processes happen after the service, dealing with claims, payments, and collections.
Front-end RCM Processes
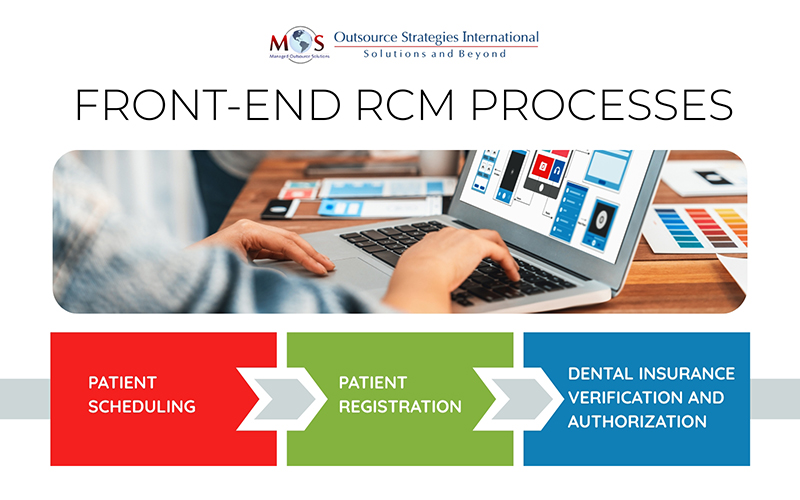
- Patient Scheduling
Dental appointment booking is an ongoing process, often done months in advance. Efficient scheduling maximizes dental professionals’ ability to maximize their time with each patient, reduces patient wait times, increases patient satisfaction.
- Patient Registration
Patient registration involves collecting and recording a patient’s information to establish a medical record and facilitate care delivery and billing. Accurate demographic details, medical history, insurance information should be collected for communicating smoothly, providing treatment, and billing services. Patients’ eligibility for insurance must be confirmed so that care can be coordinated based on coverage.
- Dental Insurance Verification and Authorization
Accurate insurance information is essential for billing purposes. Verifying insurance eligibility for new patients helps confirm active coverage, patient financial responsibility, policy limitations or exclusions, and any prior authorization requirements.
As patients’ dental coverage and benefits can change due to several factors, insurance checks for existing patients need to be done before services are provided, at each visit. If patient eligibility is not verified at the time of check-in, it can lead to errors in claim submission, denials, and lost revenue. If required by the insurer, prior authorization must be requested for services like crowns, implants, or orthodontics.
Backend RCM Processes
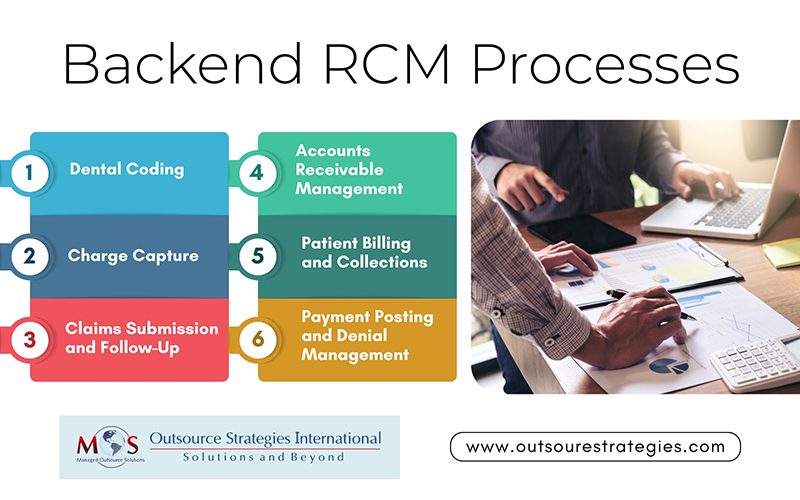
- Dental Coding
Coding is a key step in the dental RCM workflow and forms the basis for accurate billing. Accurate dental coding requires using the most specific and up-to-date CDT code to reflect the procedure performed. Even small dental coding errors can trigger claim denials, revenue loss, or audits. Common issues include incorrect CDT code selection, unbundling procedures, and inadequate documentation of medical necessity. With CDT codes updated annually and payer rules constantly evolving, practices need to keep an eye out for any changes that may have taken place such as the new, deleted, revised codes.
- Charge Capture
After accurate dental coding is completed to represent procedures performed, the next critical step is charge capture — entering the coded services into the practice’s billing system. Charge capture involves accurately documenting and recording all billable services, treatments, procedures, medications, and supplies provided to a patient during their visit. This step ensures that documentation supports billed procedures and that all dental services are reflected in the patient’s claim or invoice. Accurate charge capture ensures the practice is reimbursed for all services provided, minimizing lost revenue due to undocumented services or coding errors. In a dental billing company, billing specialists leverage advanced technology and specialized software to automate the claim generation process, minimizing human error and ensuring accuracy.
- Claims Submission and Follow-Up
When charge capture is complete, the billing system generates a claim, which is sent to the payer for reimbursement. Generating clean claims with all the required information and conforms to payer policies is an essential aspect of effective dental RCM workflow. In dental billing, claim validation or scrubbing is the back-end counterpart to insurance verification. It involves rechecking patient demographics and insurance details before submitting a claim. Automating this step ensures accurate data is used, helping prevent claim denials due to coverage or demographic errors—ultimately improving the dental practice’s financial performance. Timely claim submission is crucial to meet payer deadlines and ensure prompt reimbursement.
- Accounts Receivable Management
Efficient A/R management in the dental RCM workflow ensures timely follow-up and collection of outstanding patient and insurance balances. The most effective way to manage accounts receivable (AR) is by setting clear financial policies, keeping accurate records, following up quickly on unpaid invoices, and maintaining open communication with patients to resolve outstanding balances. If fee collection is slow or difficult, the American Dental Association (ADA) recommends reviewing your financial policies and patient payment information. Clearly outline staff procedures for handling overdue accounts, including documenting patient payment promises. Track overall and payer-specific average days in A/R to spot delays and address billing inefficiencies for faster payments.
- Patient Billing and Collections
Efficient dental patient billing is crucial for a healthy RCM workflow. Ensure patient forms explain their responsibility to pay before or at treatment. Ensure clear, written financial policies that outline payment expectations, accepted payment methods (such as credit cards, digital wallets, financing), payment plans, and collection procedures. Provide patients with detailed cost estimates before procedures, clearly explaining what insurance is expected to cover and their estimated out-of-pocket costs. During consultations, openly discuss various payment options to address patient concerns about costs. Clear, well-communicated financial policies are key to collecting patient payments and minimizing accounts receivable issues.
- Payment Posting and Denial Management
Payment posting and denial management are vital parts of the dental revenue cycle, ensuring accurate accounting and steady cash flow. Payment posting involves recording payments from insurers and patients, applying necessary adjustments, and reconciling accounts. Accurate and timely posting:
- Identifies payment patterns and flags underpayments, overpayments, or errors
- Maintains up-to-date financial records
- Prevents revenue loss from discrepancies or unpaid balances
- Reduces the need for re-billing, disputes, and claim resubmissions
- Reduces risk of audits by ensuring accurate payment records that comply with industry standards
By supporting clear communication with patients about their balances, accurate payment posting avoids confusion or misunderstandings.
Denial management focuses on identifying, analyzing, and resolving denied claims. It includes correcting errors, appealing denials, and implementing fixes to prevent recurring issues. Quickly addressing denials is crucial to ensure your practice receives compensation for services rendered.
- Monitoring KPIs and Continuous Improvement in Dental RCM
Tracking key performance indicators (KPIs) is essential for evaluating the effectiveness of dental RCM processes. Tracking essential Dental RCM KPIs such as Days in Accounts Receivable (A/R), Denial rate, net collection ratio, and First Pass Resolution Rate (FPRR) helps make informed decisions, streamlines processes, and ensures your dental billing system supports long-term financial stability and growth. By continuously monitoring these metrics, practices can identify inefficiencies, benchmark performance, and implement improvements that enhance financial outcomes.
Outsourcing to Streamline your Dental RCM Workflow
Building an effective dental RCM workflow is essential for maintaining financial health, ensuring timely reimbursements, and delivering a smooth patient experience. From front-end tasks like insurance verification and treatment planning to back-end processes such as payment posting and denial management, every step plays a critical role in the revenue cycle.
Streamlining the dental claims process for faster reimbursements is easier when you have the right support. Outsourcing dental RCM services can ensure efficiency by bringing in specialized expertise, advanced technology, and dedicated support. With the right outsourcing partner, your practice can improve cash flow, reduce claim denials, and stay on top of performance metrics, driving growth, efficiency, and long-term success.
Learn how our expert dental RCM services can boost your cash flow.




