Obtaining reimbursement for dental services depends on timely and accurate billing and coding, often making dental revenue cycle management a complex task. Maintained by the American Dental Association (ADA), Current Dental Terminology (CDT) codes are standardized codes that classify every dental procedure and service, such as fillings, crowns, or preventive services. Reporting current and appropriate dental procedure codes on claims is essential as CDT codes directly impact insurance payments. CDT coding errors delay insurance payments and disrupt a dental practice’s cash flow.
Commonly Used CDT Codes
Accurate CDT coding directly affects how much and how quickly a dental practice is reimbursed. Practices should watch out for errors when using these common CDT codes:
Preventive Procedures
D0120 – Periodic oral evaluation
D0150 – Comprehensive oral evaluation
D1110 – Prophylaxis (cleaning) – adult
D1120 – Prophylaxis – child
D1206 – Topical fluoride varnish
D1351 – Sealant (per tooth)
Restorative Procedures
D2140 – Amalgam filling, one surface, posterior
D2150 – Amalgam filling, two surfaces, posterior
D2160 – Amalgam filling, three surfaces, posterior
D2330 – Resin-based composite, one surface, anterior
D2331 – Resin-based composite, two surfaces, anterior
D2332 – Resin-based composite, three surfaces, anterior
Endodontic Procedures
D3310 – Root canal, anterior tooth
D3320 – Root canal, premolar
D3330 – Root canal, molar
Periodontal Procedures
D4341 – Scaling and root planing, four or more teeth per quadrant
D4342 – Scaling and root planing, one to three teeth per quadrant
D4910 – Periodontal maintenance
Prosthodontic Procedures
D5110 – Complete denture, maxillary
D5120 – Complete denture, mandibular
D5213 – Partial denture, maxillary, resin base, metal framework
D5214 – Partial denture, mandibular, resin base, metal framework
Oral Surgery Procedures
D7140 – Extraction, erupted tooth or exposed root
D7210 – Surgical removal of erupted tooth
D7220 – Surgical removal of impacted tooth, soft tissue
D7230 – Surgical removal of impacted tooth, partially bony
D7240 – Surgical removal of impacted tooth, completely bony
Crown and Bridge Procedures
D2740 – Crown – porcelain/ceramic substrate
D2750 – Crown – porcelain fused to high noble metal
D2790 – Crown – full cast high noble metal
D6210 – Pontic – cast high noble metal
D6240 – Pontic – porcelain fused to high noble metal
Reduce denials and speed up reimbursements with our professional dental billing services.
How CDT Codes affect Dental Insurance Reimbursements
In dental practices, CDT codes are the foundation of accurate billing and insurance reimbursements. Insurance companies use these codes to determine coverage and reimbursement amounts. Using the correct CDT codes ensures that dental procedures are properly documented and paid for, while incorrect coding can lead to claim denials, delayed payments, or underpayments.
CDT codes impact insurance payouts in several ways:
- Claim Processing
Insurance companies use CDT codes to determine if a procedure is covered under the patient’s plan. For example, a patient requests a tooth whitening procedure and the dentist performs it, submitting the claim with:
CDT Code: D9975 – External bleaching, per arch
The insurance company reviews the CDT code D9975 and identifies it as a cosmetic procedure, which is not covered under most dental insurance plans. As a result, the claim is denied and the patient is responsible for the full cost.
If the procedure had been something like D1110 – Prophylaxis (adult cleaning), the insurer would recognize it as a preventive service and likely cover it fully or partially, depending on the plan.
- Payment Delays & Denials
If a CDT code is incorrect or doesn’t match the performed service, the claim will likely be denied, delaying payment for the practice and potentially increasing out-of-pocket costs for the patient.
Here’s an example of incorrect CDT coding that occurs when scaling and root planing (SRP) is coded as prophylaxis. Prophylaxis and SRP are distinct procedures. The key difference is that prophylaxis is for prevention and maintaining oral health, whereas SRP is a therapeutic treatment for a specific condition.
A dental hygienist performs scaling and root planing (SRP) on a patient with generalized moderate periodontitis. However, the claim is mistakenly coded as:
D1110 – Prophylaxis, adult
The correct code for SRP is D4341 – Periodontal scaling and root planing, four or more teeth per quadrant (or D4342 if one to three teeth per quadrant are treated). Prophylaxis CDT code D1110 is used for a routine cleaning (removal of plaque, calculus, and stains) in patients without active periodontal disease.
The claim will likely be denied because the documentation and diagnosis (periodontal disease) do not match the preventive code submitted. It may also delay payment and raise compliance issues if such mismatches occur frequently.
- Revenue Loss due to Expensive Claim Rework
Denied dental insurance claims lead to lost revenue, as practices must spend time resubmitting them and navigating appeals processes. According to Medical Group Management Association (MGMA), it costs physician practices approximately $25-$30 to rework a denied claim. This figure represents the average expense associated with staff time, resources, and administrative workload required to address and resubmit claim denials for payment. This cost adds up quickly when many claims are denied or require resubmission. For example, a single physician practice reworking 99 denied claims per month at $25 each faces an annual cost of nearly $30,000.
- Fraud Risk – Upcoding and Downcoding
Using codes that are higher or lower than the service provided (upcoding or downcoding) can be considered insurance fraud and may lead to audits, fines, and legal action. Here are examples showing both upcoding (using a higher-level code) and downcoding (using a lower-level code) in dental billing:
Upcoding: A dentist places a one-surface amalgam filling on a molar but submits the claim using D2150 – Amalgam, two surfaces, posterior. The procedure should be coded as D2140 – Amalgam, one surface, posterior. Submitting D2150 is upcoding as it overstates the complexity and cost of the service.
The claim may lead to an audit, penalties for upcoding or denial if documentation doesn’t support the higher code.
Downcoding: if the dentist performs a three-surface composite filling but codes it as D2391 – Resin-based composite, one surface, posterior. The correct code is D2393 – Resin-based composite, three surfaces, posterior. Submitting D2391, a lower-level code, reduces reimbursement below what was legitimately earned.
Summing up, the impact of coding errors in dental claims includes:
- Underpayment: Using a lower-level CDT code than the procedure performed → lower reimbursement.
- Overpayment: Submitting a higher-level code than warranted → potential audits, recoupments and legal action.
- Claim Denials: Mismatched CDT codes, documentation errors, or plan rule violations → rejected claims.
- Revenue Loss: Reworking denials adds administrative workload and consumes staff time and resources.
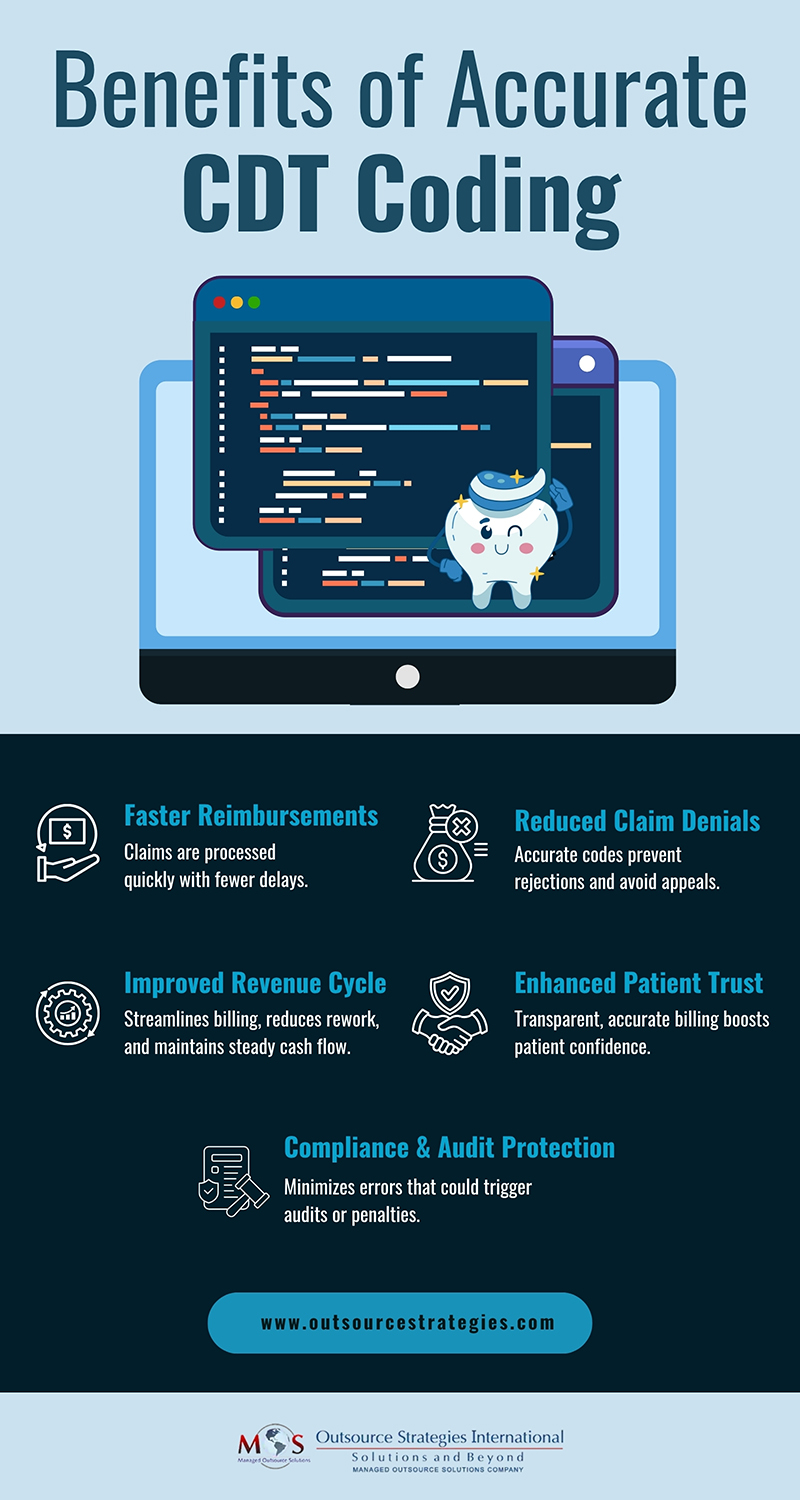
Benefits of Accurate CDT Coding
- Faster and correct reimbursements: Accurate CDT coding ensures claims are processed smoothly and payments are received without delays.
- Reduced risk of audits and claim disputes: Proper coding minimizes errors that trigger payer reviews, denials, or compliance investigations.
- Improved dental revenue cycle management: Correct coding optimize billing, reduce rework, and maintain steady cash flow.
- Minimal errors and enhanced patient trust: When billing is accurate and transparent, enhances patients’ trust in the practice.
Common Coding Challenges and Tips to Maximize Reimbursement
Common CDT coding issues can significantly affect claim outcomes and payment timelines. Using outdated CDT codes is one of the most frequent errors—since these codes are updated annually, submitting an old code can lead to immediate claim rejections. Complex procedures such as multi-surface fillings, crowns, and surgical treatments often involve multiple applicable codes, and choosing the wrong one can result in incorrect reimbursement. Documentation gaps also cause problems, as insurers require that each CDT code submitted accurately reflects the procedure described in the clinical notes.
CDT codes are the key to accurate dental insurance reimbursements. To overcome these challenges and maximize reimbursement, follow these tips:
- Stay updated with the latest CDT code changes – The ADA updates dental procedure codes every year and staying updated ensures use of the current codes.
- Ensure clinical documentation supports the CDT code submitted – To prevent claim denials and ensure proper reimbursement, make sure the procedure notes clearly match the CDT code.
- Review claims before submission to minimize errors – Carefully checking each claim helps catch coding mistakes, documentation gaps, or mismatches, reducing denials and speeding up reimbursement.
Consider using professional dental billing services – Experts can help implement best practices to ensure accurate CDT coding and dental claim processing, avoid claim denials, and maximize reimbursement.
Benefits of Professional Dental Billing for Accurate CDT coding
As a professional dental billing company, OSI ensures accurate CDT coding, which can directly improves your practice’s efficiency and revenue. Our skilled billing teams reduce errors that lead to claim denials, underpayments, or audits by verifying that each code matches the procedure and documentation. This accuracy speeds up your practice’s reimbursements, minimizes administrative workload, and enhances compliance with insurance and regulatory requirements. By ensuring billing is transparent and error-free, our support can foster patient trust and ensure better revenue cycle management, allowing you to focus more on patient care rather than chasing delayed or rejected claims.
Optimize your insurance claims today
Partner with our expert dental billing team for accurate CDT coding!




