Accurate medical billing services are vital for the financial health and operational efficiency of chiropractic practices. Chiropractors may have to treat diverse conditions such as – carpal tunnel syndrome, plantar fasciitis, epicondylitis, sprains and strains, tendinitis, fractures, ligament injuries, myelopathy, herniated discs, and more. Complete documentation of these treatments, supported by efficient chiropractic billing services, can help providers get on-time reimbursement for the services provided. With proper attention to detail, accurate coding, and comprehensive documentation, chiropractic billing professionals ensure that all services provided for musculoskeletal conditions are properly billed and reimbursed.
The coverage of treatment offered under chiropractic services is of limited benefit. The coverage is limited to subluxation or manual manipulation of the condition. Subluxation refers to the condition wherein a spinal vertebra is out of position in comparison to other vertebrae. The manual manipulation is done by following the guidelines of physical examination which include analyzing pain, asymmetry/misalignment, range of motion abnormality, and tissue/tone texture. Precise billing ensures that the services rendered are properly documented and billed, which is important for timely reimbursement and increased revenue.

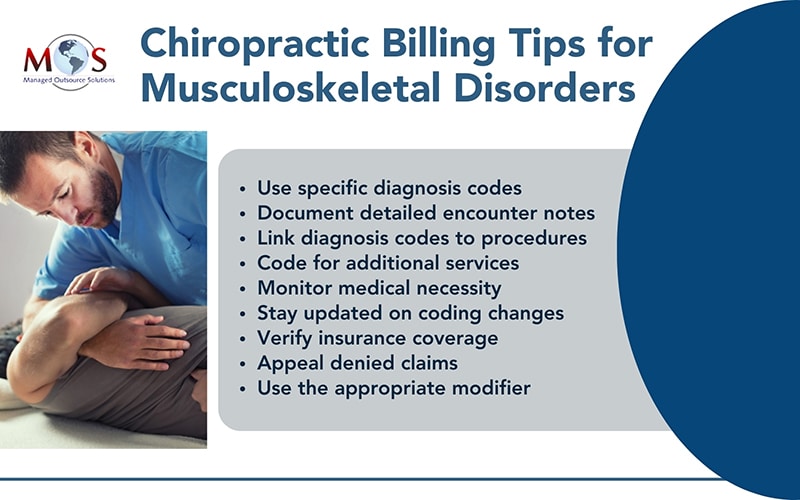
Chiropractic Billing for Musculoskeletal Disorders – Best Practices
When reporting musculoskeletal disorders, it’s essential to adhere to coding guidelines and accurately document the patient’s condition and treatment.
Here are some chiropractic billing tips for reporting musculoskeletal disorders:
- Use specific diagnosis codes: Select diagnosis codes from the International Classification of Diseases, Tenth Revision (ICD-10) that accurately describe the patient’s musculoskeletal condition. Be as specific as possible to ensure proper reimbursement and to avoid claim denials.
- Document detailed encounter notes: Provide thorough documentation of the patient encounter, including the history of present illness, physical examination findings, assessment, and treatment plan. Include details such as the location, severity, duration, and aggravating factors of the musculoskeletal disorder.
- Link diagnosis codes to procedures: Ensure that the diagnosis codes reported on the claim form are supported by the services rendered during the visit. The treatment provided should be directly related to the diagnosed musculoskeletal disorder.
- Code for additional services: Consider including additional services such as diagnostic imaging (e.g. X-rays, MRI) or therapeutic procedures (e.g. manual therapy, therapeutic exercises) when appropriate. Assign the corresponding procedure codes to accurately reflect the services provided.
- Monitor medical necessity: Verify that the services rendered are medically necessary for the patient’s condition and are supported by the documentation. Insurance payers may request additional information to justify the medical necessity of chiropractic care for musculoskeletal disorders.
- Stay updated on coding changes: Stay informed about updates to coding guidelines and changes to musculoskeletal disorder codes to ensure accurate reporting. Regularly review coding resources and attend continuing education courses to stay current with coding practices.
- Verify insurance coverage: Before providing services, verify the patient’s insurance coverage for chiropractic care and any specific requirements or limitations related to musculoskeletal disorder treatments. This helps prevent claim denials and ensures proper reimbursement.
- Appeal denied claims: If a claim is denied, review the denial reason and documentation thoroughly. If the denial is unwarranted, submit an appeal with additional supporting documentation to contest the decision and request reconsideration.
- Use the appropriate modifier: Modifiers provide additional information to payers about the services rendered, ensuring that the claims are properly processed and reimbursed. For musculoskeletal disorders, modifiers such as -LT (Left side), -RT (Right side), and -59 (Distinct Procedural Service) may be necessary to indicate specific treatments or procedures performed on different areas of the body or during separate encounters. Additionally, modifiers can clarify the complexity of services provided, such as -25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service), which distinguishes evaluation and management services from procedures.
By following these chiropractic billing tips for reporting musculoskeletal disorders, chiropractors can ensure accurate coding, proper documentation, and timely reimbursement for the services provided to patients.
Why Should You Outsource?
By partnering with a specialized billing service, chiropractors can benefit from services of dedicated billing professionals who understand the complexities of chiropractic coding, regulations, and compliance requirements. Outsourcing eliminates the need for in-house billing staff, reducing overhead costs associated with salaries, training, and benefits. Moreover, a professional chiropractic billing company will invest in advanced billing software and technology, ensuring accurate claim submission, faster reimbursement, and fewer billing errors.