The National Institutes of Health (NIH) concluded that over 20% of Americans (57.8 million) live with some form of mental illness.
Treatments include various forms of psychotherapy, medications, psychosocial interventions and other modalities such as electroconvulsive therapy or ECT, based on each patient’s needs. However, while they strive to provide quality mental health services, submitting claims for reimbursement is a major challenge due to the variety in the types of services and numerous coding and billing rules and payer regulations. Partnering with a psychiatry/mental health medical billing company can help practitioners file accurate claims and get paid appropriately and faster.
Here are some key things to note to precisely code and bill mental health services.


Remove the stress of mental health coding and billing by partnering with our specialized team of professionals!
Behavioral Health Billing Considerations
- Duration of visit – Mental health treatment such as psychotherapy sessions are usually held for a duration of 40 to 60 minutes per patient on a weekly basis. Therefore, the coding values vary significantly with changes in time length.
- Service limit – Insurance payers may place limitation on the number of sessions that are covered in a health plan. So, it is crucial to verify eligibility before a session is assigned to a patient.
- Special codes – Mental health billing requires nuanced understanding of Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and Evaluation and Management (E/M) codes.
- Customized treatment – There isn’t a one-size-fits-all treatment option when it comes to mental health.
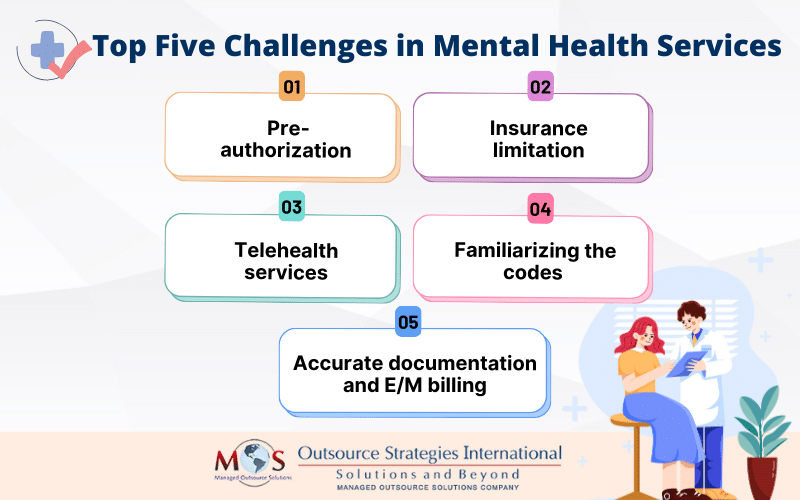
Challenges of Billing Mental Health Services
Psychiatrists treat diverse conditions such as anxiety, depression, schizophrenia, bipolar disorder, anorexia, substance abuse, ADHD, OCD, and PTSD. Proper reimbursement depends on accurate procedure coding. Coding errors can lead to late payments or claim rejections. The billing process involves completing an intake assessment that covers all the information needed to manage the patient’s billing during the care process. Submitting insurance claims can be a major challenge due to the variety in the types of services and numerous coding and billing rules and payer regulations. Partnering with a psychiatry/mental health billing company can help practitioners file accurate claims and get paid appropriately.
- Pre- authorization
Healthcare plans may require prior authorization before approving patients for mental health services, adding to the complexity of mental health billing. Verifying coverage and patient eligibility is critical to obtain approval before providing treatment or certain medication for ensuring the professionals are paid adequately. The coverage given varies based on the services rendered and policies of the insurance provider. This is a taxing, time-consuming process which could delay access to necessary patient care and interrupt healthcare providers’ decisions regarding care for their patients, so it is vital that you clearly understand the pre-authorization requirements. Delegate this task to an insurance preauthorization company for efficient and prompt payment to minimize delays in care delivery and optimize patient outcomes.
- Insurance limitations
It can be difficult to convince payers that the treatment prescribed was appropriate for the patient. Insurers usually have restrictions about the number of sessions that can be billed per day.
The rules and regulations regarding mental healthcare vary from one insurance payer to another. Payers impose maximum time limits and visitation counts eligible for treatment on a weekly, monthly or yearly basis for a patient. Some payers do not cover mental health services and patients may have to pay out of pocket for this service. You must adhere to every distinct criteria laid down in order to authorize your claims. Outsource your insurance verification and authorization to an insurance verification company to provide transparency, stabilize and safeguard your entire insurance process.
- Telehealth services
The Consolidated Appropriations Act 2023 extended Medicare telehealth flexibilities until December 31st 2024. So, the 6-month in-person visit requirement eligibility before a patient can access telehealth services is delayed. This means that behavioral care professionals can provide treatment to patients regardless of geographic restriction and receive reimbursement for their services.
In addition, telehealth flexibilities for Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) are extended so patients living in rural and underserved areas have access to behavioral health services as well. Despite the advancements, there exist certain challenges, including:
- Limited mental health provider-patient contact that may affect patient assessment
- Variation in the quality of audio and video call, such as poor sound or visual between provider and patient
- Concerns of privacy since sensitive patient information is involved
- Coding Difficulties
Proper reimbursement depends on accurate procedure coding. Coding errors can lead to late payments or claim rejections. Frequent errors can attract audits, or even charges of fraud and abuse, resulting in elimination from managed care networks. Physician coding service providers always verify CPT codes with the AMA’s latest CPT manual to ensure correct and up-to-date procedure codes. There are specific codes assigned in CPT and HCPCS codes to bill for behavioral health services. The set of behavioral healthcare codes under Current Procedural Terminology (CPT) and the Healthcare Common Procedural Coding System (HCPCS) includes:
- CPT codes that are reimbursable for mental health when billed with modifier “95”:
-
- 90832: (individual therapy, less than 30 minutes)
- 90834: (individual therapy)
- 90837: (individual therapy, longer duration of minimum 53 minutes)
- 90791: (initial client assessment)
- 90792: Psychiatric diagnostic evaluation (with medical services)
- 90846: Family psychotherapy (without patient present)
- 90847: Family psychotherapy (with patient present)
- 90853: Group Psychotherapy (not family)
- 96156: Health behavior assessment
- 96158: Health behavior intervention (individual,30 minutes)
- 96159: Health behavior intervention (individual, additional 15 minutes)
- 96164: Health behavior intervention (group, 30 minutes)
- 96167: Health behavior intervention (family, with patient present)
- 96168: Health behavior intervention (family, with patient present, additional 15 minutes)
- HCPCS Codes
- G0017: Psychotherapy for crisis furnished in an applicable site of service (any place of service at which the non-facility rate for psychotherapy for crisis services applies, other than the office setting); first 60 minutes
- G0018: Psychotherapy for crisis furnished in an applicable site of service (any place of service at which the non-facility rate for psychotherapy for crisis services applies, other than the office setting); each additional 30 minutes
- G0019: Community health integration services performed by certified or trained auxiliary personnel, including a community health worker, under the direction of a physician or other practitioner; 60 minutes per calendar month
- G0022: Community health integration services, each additional 30 minutes per calendar month
- G0136: Administration of a standardized, evidence-based social determinants of health risk assessment tool, 5-15 minutes
Marriage and Family Therapists (MFTs) and Mental Health Counselors (MHCs) are now able to directly enroll for Medicare reimbursement by incorporating the new codes into your billing system.
- POS (Place of Service) Codes:
- POS 02: Telehealth provided other than in patient’s home is paid at the facility rate.
- POS 10: Telehealth provided in patient’s home is paid at the non-facility rate.
-
- Accurate documentation and E/M billing
Maintaining accurate documentation of each patient encounters, assessment, description of services and treatment plans, and progress notes that justify the necessity of mental health services will help you with both pre-authorization and claims appeals. Integrate EHRs into your practice to streamline your workflow, reduce errors, lessen manual paperwork and optimize billing. Employ EHRs to document the following data:
-
-
- Forms
- Progress Notes
- Assessment
- Treatment plans
-
Effective since 2024, providers should bill E/M codes according to the total length of time spent with a patient and the time must either reach or exceed the amount to use that code.
CPT codes and the 2024 minimum standard of time required to spend on a patient:
-
- 99202 – 15 minutes
- 99203 – 30 minutes
- 99204 – 45 minutes
- 99205 – 60 minutes
- 99212 – 10 minutes
- 99213 – 20 minutes
- 99214 – 30 minutes
- 99215 – 40 minutes
According to the new E/M guidelines, when a single patient is admitted to multiple visits in the same hospital/observation on a single calendar date, then a single service is recorded. However, if they are discharged and re-admitted to another department on the same day then multiple visits are reported.
The billing process also involves completing an intake assessment that covers all the information needed to manage the patient’s billing during the care process. Documentation must also provide evidence that the care is medically reasonable and necessary. Insurance benefits verification must be performed before services are provided to check the patient’s active coverage with the insurance company. This can be complex as covered benefits vary between companies and with each individual insurance plan.
With all the complexities involved, it’s clear that mental health billing and coding would be much easier with expert support. As you focus on providing the care your patients need, hiring a medical billing outsourcing company with experience in coding, pre-authorization and insurance eligibility verification, and third party billing for mental health services is a practical option to reduce the risk of denials and optimize reimbursement.


Consider partnering with OSI for smoother mental health billing and coding processes.