Medicaid programs are predominantly aimed at covering dental services for children and youth under the age of 21. There are certain states that give adult dental benefits. However, there is no health coverage for orthodontic treatments that are rendered for cosmetic reasons. Medicaid provides coverage benefits only for orthodontic procedures that are a medical necessity. Poor oral health is a cause of concern in the United States and it particularly impacts people with low incomes. Taking this into consideration, Medicaid provides dental services such as check-ups, cleanings, fillings, and extractions. For example, Early and Periodic Screening, Diagnostic and Treatment benefit (EPSDT) is Medicaid’s comprehensive child health program.
Medical necessity
Medical necessity is an important factor for a patient to be eligible for Medicaid-reimbursable therapy and treatment services. The definitions of medical necessity in states are based on certain constraints and they vary from state to state. Some states reduce Medicaid costs by having cost restrictions in place. This is done by limiting patients to the least expensive treatments. One of the common restrictions on states’ definitions of medical necessity is prohibitions against experimental treatments. Whereas in some states, the definition of medical necessity is broad. The opinion of orthodontists that are pertinent to the medical condition is taken into consideration.
Applicability of Medicaid coverage in some common dental problems
As mentioned above, the dental problems that are covered under Medicaid programs differ from state to state. Here are two important orthodontic procedures and the applicability of their Medicaid coverage.
Dental Anesthesia procedure:
With reference to ND Medicaid dental manual, the following procedures are reimbursed in North Dakota
- D9222: Deep sedation/general anesthesia -first 15 minutes
- D9223: Deep sedation/general anesthesia -each 15-minute increment
- D9239: Intravenous moderate (conscious) sedation/analgesia-first 15 minutes
- D9243: Intravenous moderate (conscious) sedation/ analgesia- each 15-minute increment
Dental anesthesia procedures have to be documented accurately in states that provide Medicaid coverage for the same. Dental practices can rely upon dental billing companies for error-free compilation of dental codes that are eligible for reimbursement.
Dental benefits of children and Medicaid coverage programs with reference to Medicaid.gov
- In most states, the medical bills for dental procedures of children are extensively covered. As per Medicaid.gov, the dental services of all child enrollees of Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit are covered.
- Oral screening is a part of a physical exam but it doesn’t substitute for a dental examination performed by the dental practice.
- The dental service for children must minimally include:
- Relief of pain and infections
- Restoration of teeth
- Maintenance of dental health
- The EPSDT mandates that all services must be provided if they are a medical necessity. Medical necessity is decided by states.
- If a condition is diagnosed during dental screening, the state is required to provide all the necessary services to treat that condition, regardless of their inclusion in the state’s Medicaid plan.
- Dental services are not limited to emergency services for children entitled to EPSDT.
- Dental services have to be provided at intervals that meet reasonable standards of dental practice. In such intervals with regard to medical necessity, the existence of suspected illness or condition has to be determined.
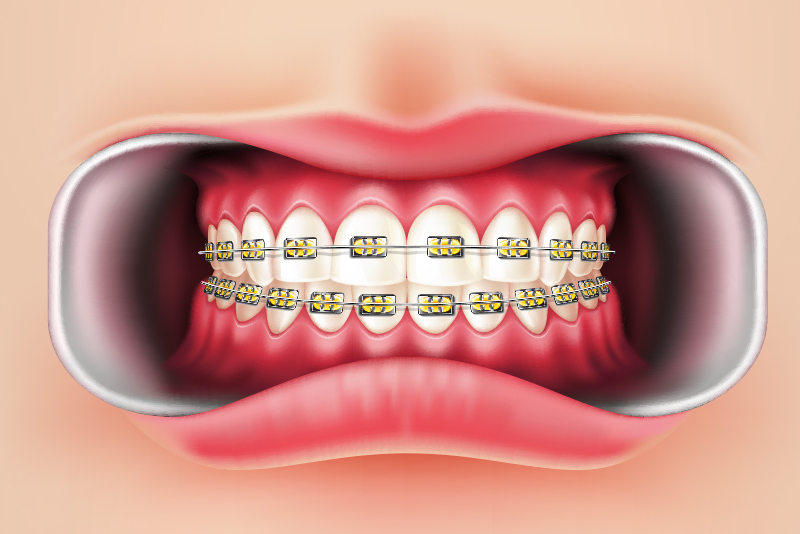
Medicaid coverage for braces for children
Dental braces – Orthodontic codes
- D8210: Removable appliance therapy
- D8220: Fixed appliance therapy
- D8060: Interceptive orthodontic treatment of the transitional dentition
- D8080- Comprehensive orthodontic treatment of the adolescent dentition
If braces are deemed a medical necessity for the child, they will be covered under Medicaid Program. An orthodontist or dentist confirms if braces are medically necessary for the child. According to mykoolsmiles.com, below given are some of the considerations that are used to determine medical necessity:
- Cleft palate
- Structural jaw issues making it difficult to open your mouth
- Issues with eating or chewing normally
- Issues with eating or chewing normally
- Issues with speech impediments from tooth or jaw problems
- Any extreme underbite, crossbite, or overbite
- Overjet teeth -When teeth protrude outwardly and sit over the bottom teeth
- Impacted teeth with an eruption
- Missing teeth due to hereditary conditions (like hypodontia)
The services provided by dental practices have to be documented correctly to eliminate claim denials. A dental billing company can assist dental practices in assigning appropriate dental codes in accordance with the Medicaid plan of the state concerned.