Billing for dental services can be a complex process due to the need to understand specific CDT codes, and navigate varying insurance plans, payer policies, and changing regulations. While outsourced dental billing services can effectively address these challenges, dentists must still stay informed about billing errors that could affect their financial health. One dental billing problem that leads to lost revenue for dental practices is bundling in dental claims. Bundling happens when insurance companies group multiple dental procedures under a single code and reimburse only one fee, instead of paying for each procedure individually.
Struggling with bundled claims?
Our dental RCM experts help you maximize reimbursements.
What Is Bundling in Dental Claims?
The American Dental Association defines bundling as “The systematic combining of distinct dental procedures by third-party payers that results in a reduced benefit for the patient/beneficiary.”
Bundling is grouping multiple dental procedures under a single code, typically when those procedures are done together. Although there are some situations where bundling is appropriate, the problem is when procedures, which are legitimately separate, are bundled either inappropriately or due to contractual provisions, without explanation. Instead of paying for each procedure individually, the payer reimburses only one fee, leading to reduced benefits for the patient and lower reimbursement for the dentist.
When does bundling occur? Payers may apply bundling based on different aspects:
- Payer policy edits: Insurance companies have proprietary internal rules and automated claims review systems known as policy edits. These edits are designed to detect and prevent what the payer deems unnecessary or overlapping billing. For example, based on frequency limitations, a payer’s system may automatically reject or bundle multiple X-rays performed on the same day—even if they were necessary. Most dental insurance plans cover just one complete set of mouth radiographs every five years—and individual X-rays, by number or type, rarely meet the criteria for a full-mouth series (ADA).
- CDT coding rules: Comprehensive CDT codes already include related services within the same code description. Core buildup (D2950) is often a necessary prerequisite to placing a crown (D2740) when a significant portion of the tooth structure is missing. Some insurance companies may bundle the buildup with the crown, so submitting both may trigger bundling. Here are some other examples of bundling in dental claims provided by the ADA, where payers may regard combinations of services inconsistent with the code:
- Pins reported as a separate service from a core buildup (the D2950 buildup code includes pins);
Adhesives, bases or liners as a separate service from the restorations (the code defines these to be included as part of the restoration); D2140 – an amalgam restoration (filling) on one surface of a tooth includes the preparation of the tooth (drilling out the decay), any necessary bonding agents, liners, or bases, and the placement and shaping of the amalgam filling. - Occlusal adjustments and minor adjustments to prostheses as a separate service, when the prosthetic service includes routine post-delivery care;
- Suture removal, as a separate service from the extractions , which include suturing and postoperative care; (D7210 for surgical removal of an erupted tooth, includes the placement and removal of sutures as well as limited bone smoothing, closure, and routine follow-up).
- X-rays taken during the course of root canal therapy as a separate service from the root canal, which by definition, includes intra-operative X-rays (D3310-D3330 for the initial root canal and D3346-D3348 for retreatment include the necessary intra-operative radiographs taken during the root canal procedure).
- Pins reported as a separate service from a core buildup (the D2950 buildup code includes pins);
-
- Perceived procedure overlap: Insurers may bundle procedures simply because they appear to be part of the same treatment session or an extension of one another, even if they were performed separately and are billable separately. For example, when a full-mouth X-ray (D0210) and bitewings (D0274) are performed on the same day, the payer may perceive them as overlapping, leading to bundling. Likewise, separate surgical extractions (e.g., D7210) may be bundled under a comprehensive extraction code (D7140).
Many payers consider core build-ups to be included in the crown procedure, even though the CDT Code lists them as separate services. It’s important to note that not every crown requires a build-up, which makes understanding proper documentation and coding essential to avoid bundling issues.
Why Is Bundling a Problem?
- Revenue loss: The bundled payment often results in less insurance reimbursement than if each procedure were billed separately. Dentists may not be compensated for all the work performed.
- Claim denials: Improper bundling can lead to claim rejections, payment delays, audit risks, and potential penalties.
- Significant operational costs: Appealing bundled dental insurance claims requires significant staff time and effort dedicated to reviewing denials, researching reasons, gathering documentation, preparing appeal letters, and communicating with payers.
- Patient confusion: Patients might not understand why distinct procedures they believe were performed separately, like multiple X-rays, are bundled into a single benefit code. When they receive the Explanation of Benefits (EOB), bundling by insurance companies can appear confusing and may result in reduced benefits, leaving them with higher than anticipated out-of-pocket expenses due to limited insurance coverage.
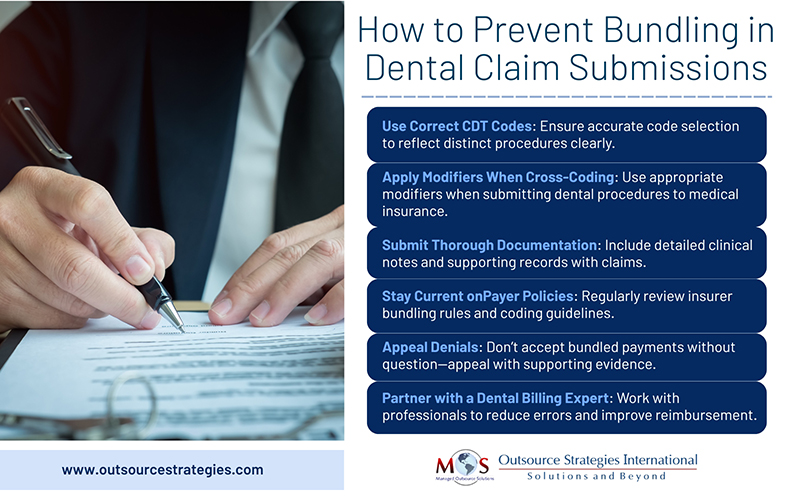
How to Prevent Bundling in Dental Claim Submissions
Using accurate and updated CDT codes, submitting comprehensive documentation about services rendered and understanding payer policies are key for avoiding dental claim denials due to bundling
Use Correct CDT Codes
CDT codes have evolved to clearly define the scope of dental procedures, even clarifying component services that may be considered part of another procedure code. Accurate understanding of CDT definitions helps avoid billing for services that are not separately reimbursable. Further, it is important to utilize the most current version of CDT and billing guidelines. The ADA points out: “One of the most common problems that payers have with claims is the use of outdated versions of CDT”.
Apply Modifiers when Cross-coding Dental Procedures to Medical Claims
While CDT codes are sufficient for standard dental procedures, modifiers are used with CPT and ICD codes to provide additional details about the service or procedure. In cases where a dental procedure might be covered by medical insurance (e.g., related to a medical condition), modifiers could be used on the CPT or ICD codes to indicate the dental service and its medical necessity.
Submit Claims with Thorough Documentation
Dentists need to provide clear clinical documentation and narratives to prove that each procedure was independently necessary and not duplicative. Include clinical notes, radiographs, and narratives to justify separate procedures.
Stay Current on Payer Policies
Each insurance company has its own bundling rules. The ADA notes that bundled services and associated payment policies can be found in the dentists’ provider manuals or online portals. Continuous staff training is crucial to maintaining compliance with bundling guidelines. Understanding payer-specific bundling policies, billing guidelines and frequency limits helps submit claims and documentation to meet these requirements. Contact payers directly to clarify concerns related to coding of dental procedures and bundling policies. Review EOBs carefully to spot bundling reductions.
Appeal Denials
If a claim is denied due to bundling, consider appealing the decision with supporting documentation and justification.
Tackle Bundling Complexities with Expert Dental Billing Support
Outsourcing dental revenue cycle management (RCM) to an expert is a practical way to avoid/tackle bundling issues. Experienced RCM partners stay up to date on payer policies, CDT coding updates, and bundling rules, ensuring that claims are submitted accurately. They are familiar with common bundling scenarios, can identify when procedures are inappropriately bundled and will appeal denials with proper documentation. By leveraging expert knowledge and technology, outsourced dental billing teams help practices maximize reimbursements.
Outsource your dental billing today and avoid costly errors caused by bundling.




