Modifiers are used in medical billing for identifying procedures that have been altered, without changing the core meaning of the code(s) submitted. Proper modifier use is crucial in claims submitted for chiropractic treatment. Many providers leverage chiropractic billing and coding services to ensure services are reported using the correct codes and modifiers, prevent claim denials, and maximize reimbursement. When it comes to modifier use in chiropractic, knowing each payer’s specific requirements is crucial.
Learn how our chiropractic medical billing and coding services can boost your practice’s efficiency.
Billing Chiropractic Manipulative Treatment (CMT): Modifier Use
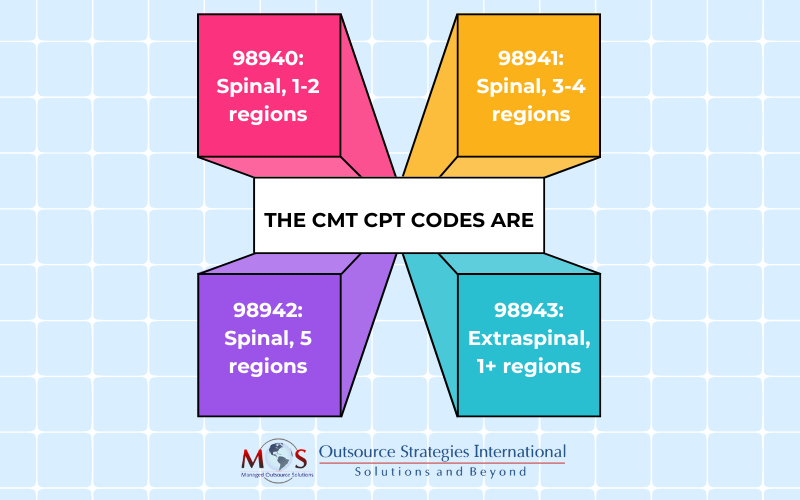
The five spinal regions for chiropractic manipulative treatment (CMT) are: cervical, thoracic, lumbar, sacral, and pelvic regions. Extraspinal regions include the head (excluding atlanto-occipital joint), lower and upper extremities, rib cage (excluding costotransverse and costovertebral joints), and abdomen.
Let’s see how modifiers 25 and 59 can be applied when reporting CMT:
- Modifier 25 Significant, Separately Identifiable Evaluation and Management Service by the Same Provider or Other Qualified Healthcare Professional on the Same Day of the Procedure or Other ServiceCMT codes include a pre-manipulation patient evaluation. Modifier 25 should be used only when the chiropractor performs an assessment above and beyond the manipulation. Some insurance companies do not cover CMT and E/M on the same day. On the other hand, some payers may pay E/M services for a new patient (99201-99205) not for an old patient (99211-99215). Providers should check commercial and federal payer guidelines when using modifier 25.
- Modifier 59, Distinct Procedural ServiceIn some cases, providers may need to report a procedure or service as independent from other non-E/M services. This requires indicating it as a separate service on the claim. Modifier 59 is used to indicate procedures or services, excluding E/M services that are typically not reported together but are appropriate in specific situations.
For example, if a chiropractor performs mechanical traction (CPT code 97012) and manual therapy (CPT code 97140) on the same day, modifier 59 would be appended to 97140 to indicate that these services are separately payable.
- Modifiers XE, XS, XP, and XU: These are four subsets of Medicare’s chiropractic billing modifiers can be used in lieu of modifier 59:
- XE: Separate Encounter, a service that is distinct because it occurred during a separate encounter.” Only use XE to describe separate encounters on the same DOS.
- XS: Separate Structure, a service that is distinct because it was performed on a separate organ/structure.
- XP: Separate Practitioner, a service that is distinct because it was performed by a different practitioner.
- XU: Unusual Non-Overlapping Service, the use of a service that is distinct because it does not overlap usual components of the main service.
CMS states: “The use of modifier 59 or XS is appropriate for different anatomic sites during the same encounter only when procedures (which aren’t ordinarily performed or encountered on the same day) are performed on different organs, or different anatomic regions, or in limited situations on different, non-contiguous lesions in different anatomic regions of the same organ.”
- AT Modifier
The Active Treatment (AT) modifier aims to clearly distinguish between active treatment and maintenance treatment. An AT modifier must be used in a claim when providing active/corrective treatment to treat acute or chronic subluxation. Medicare covers only active therapy for subluxation, and does not cover maintenance therapy. Adding AT to the CMT codes indicates that the treatment is considered “medically necessary”. However, Medicare has the authority to deny claims if deemed appropriate after a thorough review.
Improve Cash Flow with Proper Modifier Use
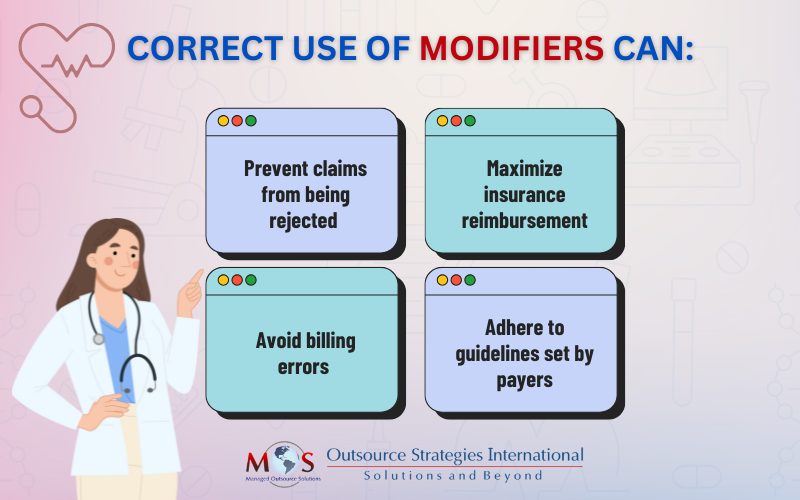
Missing modifiers, misplaced modifiers, or invalid modifier combinations are common reasons for claim denials in chiropractic care. Misusing chiropractic billing modifiers could also trigger audits, resulting in penalties. To use modifiers correctly in chiropractic, understand each payer’s specific recommendations.
Documentation should properly reflect key elements such as evaluation, a treatment plan, medical necessity and/or contraindications to treatment.
Understanding and effectively using codes and modifiers is essential for successful chiropractic medical billing. Partnering with a reliable chiropractic medical billing company can enhance efficiency and compliance, allowing providers to focus on patient care while optimizing their revenue cycle.
Maximize your reimbursements and minimize your stress with our chiropractic billing services!




