Dental billing is the process of submitting and managing claims for dental services provided to patients. Ensuring efficiency in the process is a critical aspect of managing a dental practice efficiently and obtaining proper reimbursement. Dental practitioners, office managers, and billing staff need to understand dental billing basics in order to navigate the complex world of insurance claims, coding, and reimbursement.

For a thriving practice, dental professionals must understand how dental billing works
In this dental insurance billing guide, we cover the fundamental aspects of dental billing, including patient registration, insurance verification, coding, treatment documentation, claims submission, and best practices for maximizing revenue.


Optimize your revenue cycle with our dental billing services!
Unlock your practice’s potential!
Call Today!
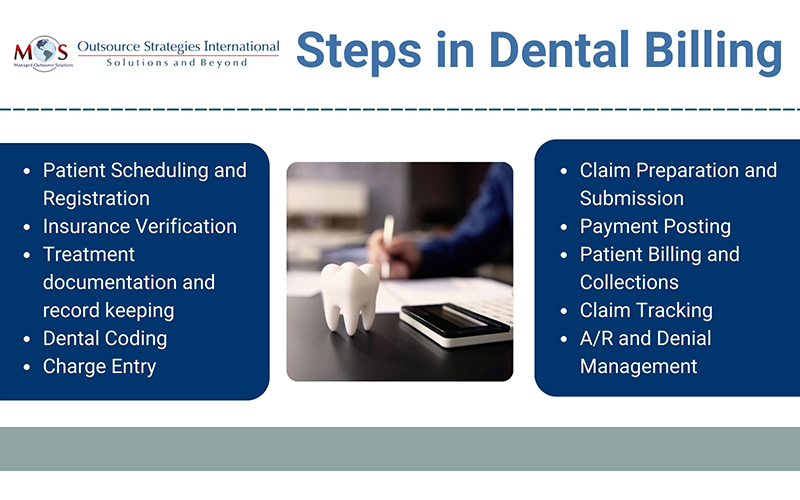
Understanding the Steps in the Dental Billing Process
Dental billing covers a series of steps aimed at obtaining payment from both insurance providers and patients for the dental services provided. While billing procedures can vary depending on insurance plans, state regulations, and individual dental practices, the basic steps are the same. Let’s delve into these steps and their significance.
Patient scheduling and registration
This is the first step in the dental billing process. The process involves booking and managing appointments for patients. When patients call to schedule their appointment, our team will meticulously collect and document vital demographic information, insurance particulars, and relevant dental history. Precision in registration is paramount for creating comprehensive and current patient profiles, promoting seamless communication among healthcare practitioners, and ensuring precise billing. Incorrect insurance details on a registration form can lead to billing problems for the practice and the patient.
Insurance verification
If the patient has dental insurance, it is important to verify their eligibility, coverage limits, and any pre-authorization requirements before providing treatment. Even if a patient has dental insurance, they may not be aware of their financial responsibilities, such as co-pays, deductibles, and out-of-pocket maximum. Obtaining a full breakdown of patients’ insurance coverage before their dental appointments ensures that patients understand their coverage and are financially prepared. This includes informing them about out-of-pocket expenses, such as deductibles, co-pays, and non-covered services. This proactive approach reduces the likelihood of unexpected costs and promotes financial transparency, ensuring a seamless experience for both patients and providers.
Billing staff typically verifies insurance eligibility, benefits, coverage limitations, and pre-authorization requirements by calling the insurance company or logging into their portal. The process involves comparing the insurance information provided by the patient with the insurance provider’s records. This step ensures that the patient’s policy is active and determines their eligibility for the requested service. Once it is confirmed that the data provided is accurate, the insurance verification process is considered complete.
The next step is effectively communicating insurance information to patients and setting expectations regarding coverage and out-of-pocket expenses. Engaging in discussions about insurance policies is crucial to ensure patients have a clear understanding of their financial responsibilities. By effectively and clearly communicating information about insurance eligibility, providers can not only address patients’ billing concerns but also resolve any questions or doubts they may have. This approach builds trust and confidence in the dental practice, ultimately enhancing patient satisfaction levels.
Treatment documentation and record keeping
Accurate and thorough documentation is crucial for proper billing. Insurance claims must be submitted with proof that the treatment performed was necessary for the health of the dental patient. The dentist must document the details of the treatment provided to the patient. This includes the procedures performed, the date of service, tooth numbers (if applicable), and any supporting documentation such as X-rays, intraoral photos (IOC) and clinical charts and notes. Clinical notes consist of the following essential information:
- Patient’s name and contact details
- Comprehensive and current medical history
- Details of prior and ongoing treatments
- Notes on missed appointments or any declined unscheduled treatment, including the date and relevant details
Detailed clinical notes are crucial when it comes to claim reimbursement. It ensures that the information submitted for claim reimbursement accurately reflects the services rendered, minimizing the risk of claim denials or delays due to incomplete or inconsistent documentation.
Ensuring a smooth and effective system for documenting and validating dental treatments is essential for precise billing and efficient practice management. In dental practices, an administrative team member is usually responsible for promptly updating the dental software following the provision of care and observations, and obtaining electronic signatures from the provider. It is considered a best practice to have a daily sign-off on the day sheet to consistently verify that the treatment provided in the dental chair is accurately recorded in the software and reflected on the patient’s ledger for billing purposes.
Coding Dental Procedures
Dental coding involves the use of official coding systems such as the Current Dental Terminology (CDT) and/or the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) to report dental conditions and treatments performed by a dental care team.
There is a specific CDT code that corresponds to each treatment provided, including preventive, restorative, and surgical procedures. Using the correct codes to document and communicate diagnoses, procedures, and services provided during dental visits is necessary for consistency in billing, reimbursement, and communication with insurance companies and other healthcare providers. ICD-10-CM codes communicate the dental or medical condition(s) needing treatment listed on the claim form to payers.
In certain cases, dentists may perform treatments that are classified as medical care. Such services can be billed to medical insurance and is referred to as dental medical billing. Dental procedures that medical insurance may cover include: facial pain treatments, issues related to damaged teeth, gums, and jaw after accidents or trauma, radiation therapy for cancer patients, medical conditions of the temporomandibular joint (TMJ), sleep apnea devices, dental implants and bone grafts, biopsies, and Botox injections for teeth grinding or jaw pain. Medical insurance companies require the claim form to have at least one diagnosis code.
Charge Entry
The encounter form is used to verify the procedures and why they were performed so that the patient can be charged all services. The charges are entered into the practice management system, specifying the services rendered and the associated charges. Any payments made by the patient at that time should be entered.
Claim Preparation and Submission
After accurately documenting and coding the treatment, it’s time to generate and submit claims to the insurance company or other third-party payers. When a claim is generated, a billing specialist reviews and “scrubs” it to ensure the presence and accuracy of each procedure, diagnosis, and modifier code. Claim scrubbing is a vital step that verifies the completeness of patient, provider, and visit information, ensuring that all necessary details are included in the claim submission.
Dental claims can be submitted electronically (via the practice management software) or on paper (typically using standard claim forms such as ADA Dental Claim Form). Using the current claim form is necessary to ensure compliance with insurance industry standards, ensure accuracy and efficiency in claims processing, get paid quickly, and minimize denials and appeals processing.
Patient Billing and Collections
Depending on the insurance coverage and the patient’s financial responsibility, the dental office bills the patient for any remaining balance after insurance reimbursement. This may include deductibles, co-pays, or services not covered by insurance.
Dental offices are responsible for collecting payments from patients. This requires communicating financial obligations to patients effectively and addressing questions or concerns on billing and insurance coverage. They should have clear procedures for patient billing such as collecting co-pays at the time of service or sending invoices for outstanding balances, and offering various payment methods such as cash, check, credit card, or payment plans.
Claim Tracking
Every claim’s status should be tracked on a daily basis. Follow-up with insurance companies is necessary to resolve any claim rejections, denials, or payment discrepancies. The dental office may need to provide additional information or resubmit claims if necessary.
A/R and Denial Management
After the claim is submitted, the insurance company reviews the claim for accuracy and determines the amount of reimbursement based on the patient’s coverage — the process known as adjudication. The insurance company may accept the claim and reimburse the dental office, or they may deny or partially deny the claim. That’s why it’s vital to have a specialized A/R staff that can follow up with insurance providers to handle disputed claim. Effective denial management improves the financial health of a dental practice.
Payment Posting
Payments are posted when the dental practice receives electronic remittance advice (ERAs), accompanying checks, or direct deposits. Payment posting ensures that accurate financial records are maintained. By examining financial data points and promptly addressing discrepancies, dental offices can promptly resolve any potential revenue leaks, safeguard their revenue stream, and make informed financial decisions.
Navigate Billing with Expert Support
Dental billing is a critical component of a practice’s revenue cycle management. Experience and expertise are necessary to successfully navigate all stages of the process, optimize administrative processes, maximize revenue, and ensure compliance with insurance regulations and billing standards. Our dental billing company has dedicated professionals who can handle the billing and coding processes efficiently, allowing practices to optimize reimbursement while delivering quality care to their patients.