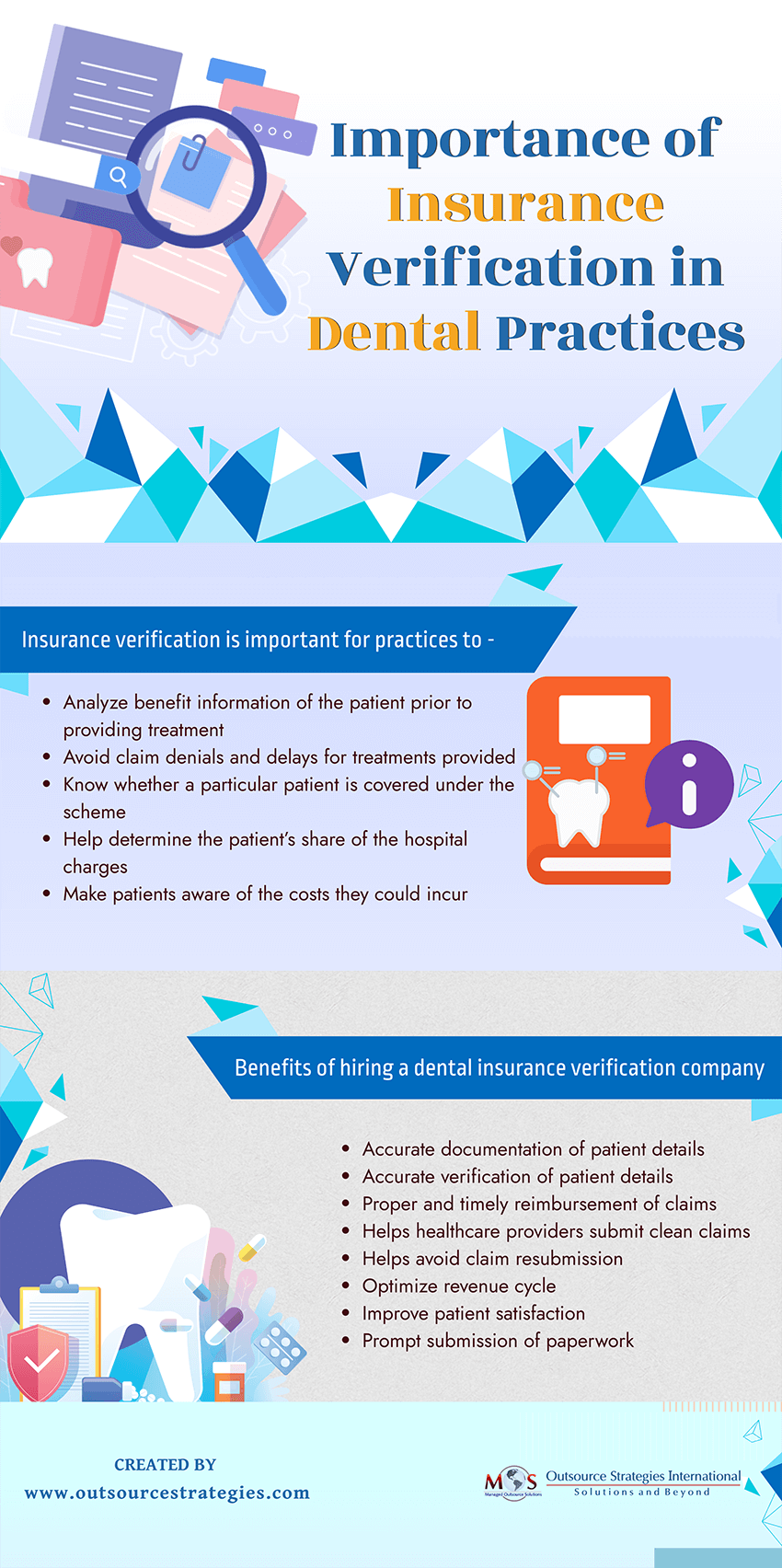
Dental eligibility verification is an important step to determine whether a patient is covered for the treatment or not. Any error or delay in verification can hamper patient retention and impact practice revenue. Practices mostly rely on professional dental insurance verification services for effective and accurate reporting of various services provided to their patients. The insurance verification process is a cumbersome task and can affect the quality of services provided by dental practices. When hiring a dental insurance verification company, dental practitioners and their staff need not divert valuable time and energy calculating patients’ benefits and claims. Reliable companies can check the eligibility of the patients with the respective insurance companies. This gives healthcare providers clarity regarding the patient’s coverage and payment obligation. This benefits both the dental practices and the patients.